Chronic conditions present a strong economic incentive for action. During the past century, a major shift occurred in the leading causes of death for all age groups, including older adults, from infectious diseases and acute illnesses to chronic diseases and degenerative illnesses. More than a quarter of all Americans, and two of every three older Americans, have multiple chronic conditions. Treatment for this chronic-conditions population accounts for 66% of the country’s healthcare budget.1
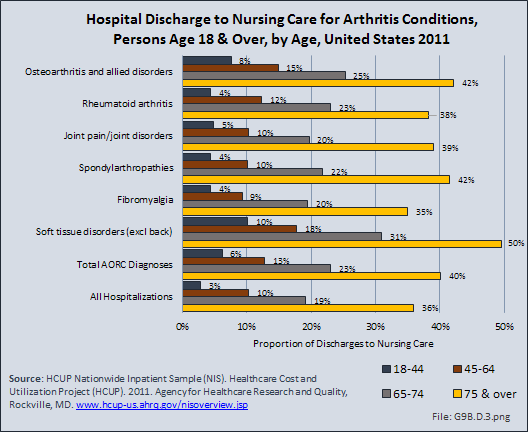
Mobility is fundamental to everyday life and central to an understanding of health and well-being among older populations. Impaired mobility is associated with a variety of adverse health outcomes. As the age of the US population continues to increase, aging and public health professionals have a growing role to play in improving mobility for older adults. There are critical gaps in the assessment and measurement of mobility among older adults who live in the community, particularly those who have physical disabilities or cognitive impairments. By changing the physical environment in which older people live and creating unique integrated interventions across various disciplines, we can improve mobility for older adults.
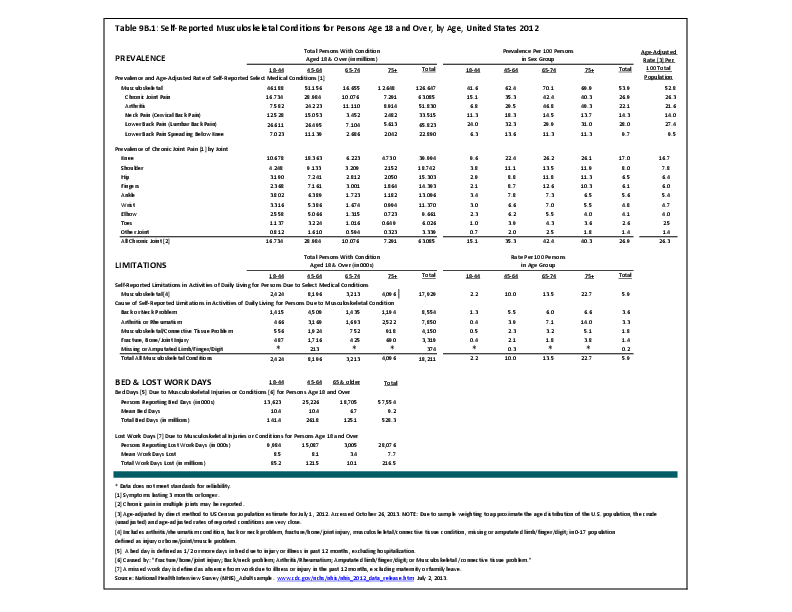
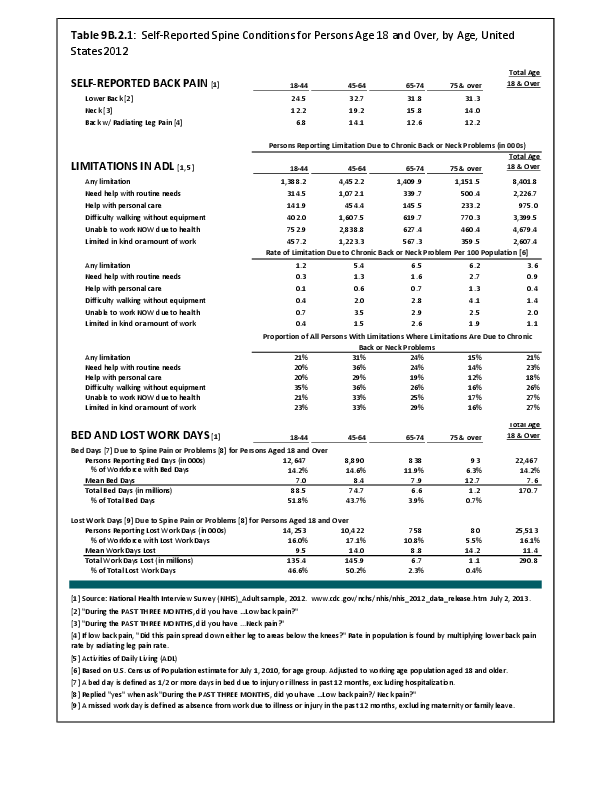
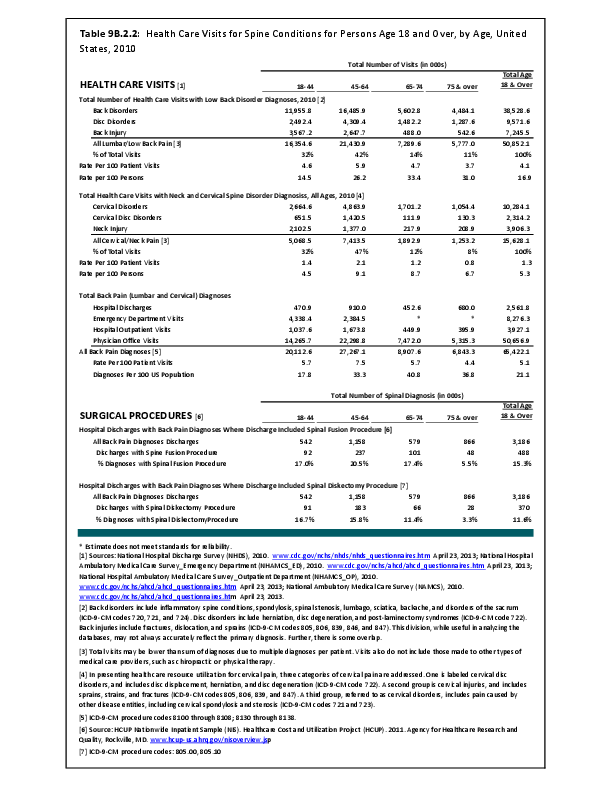
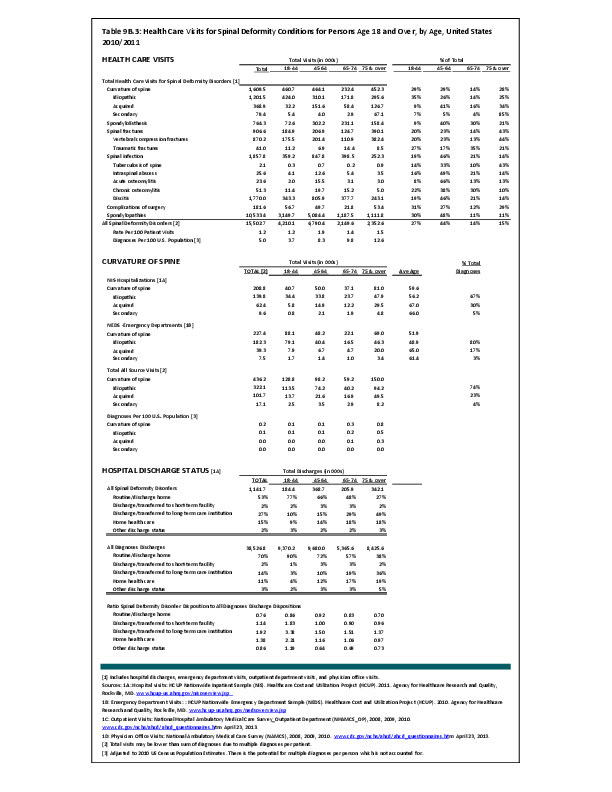
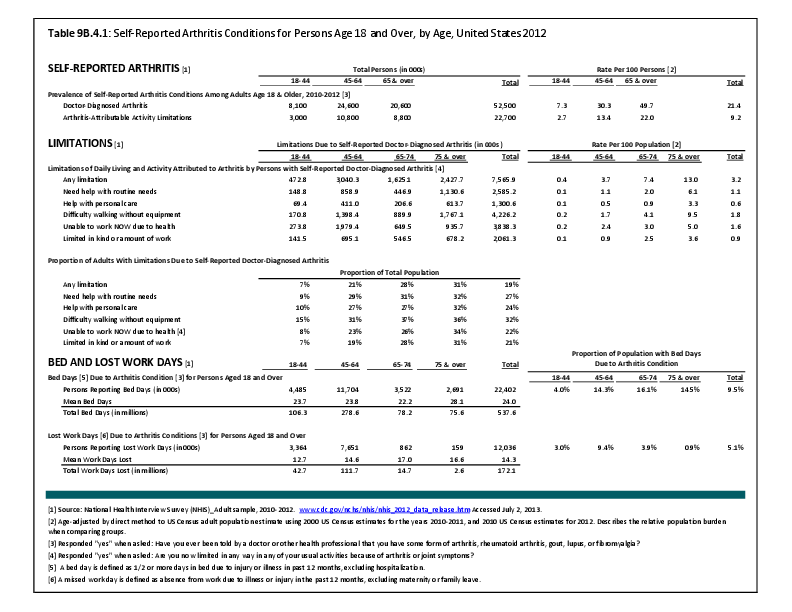
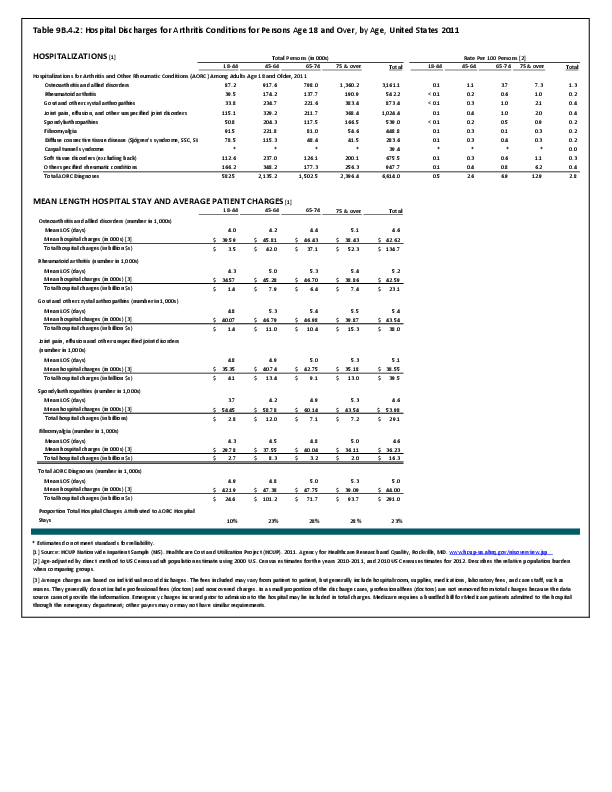
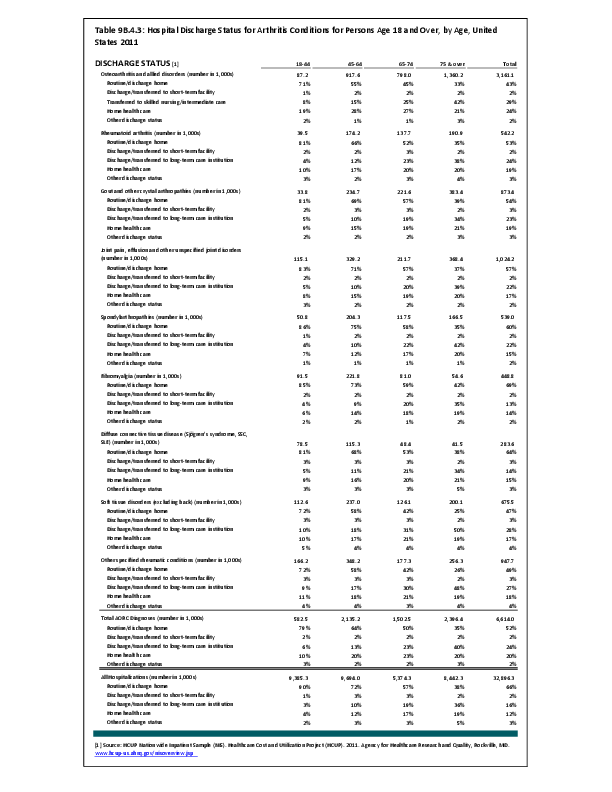
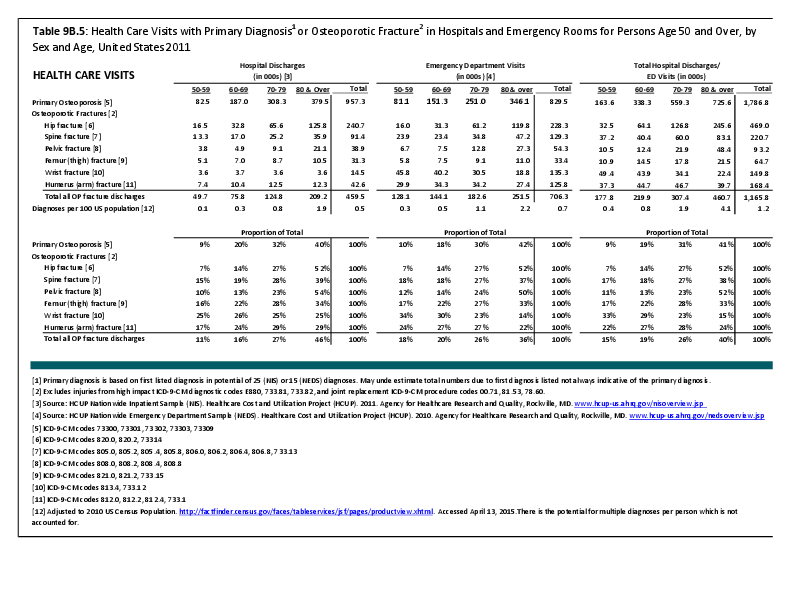
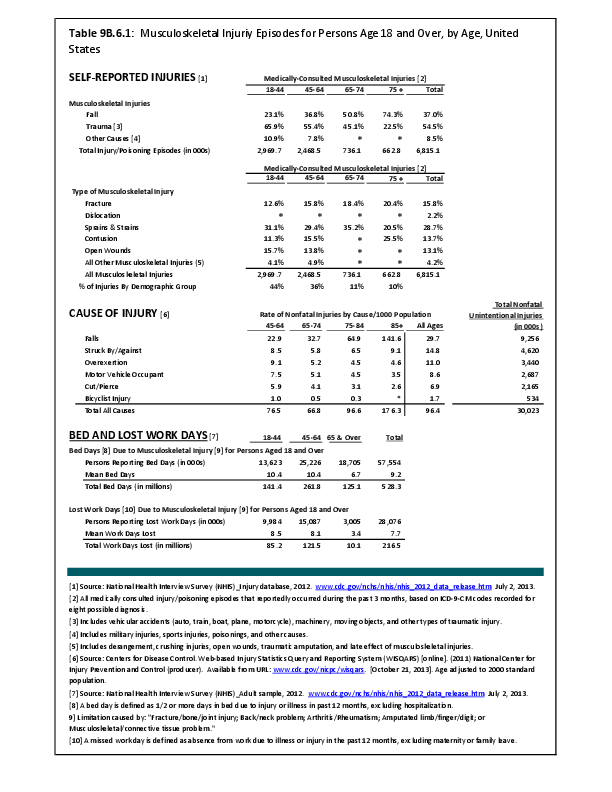
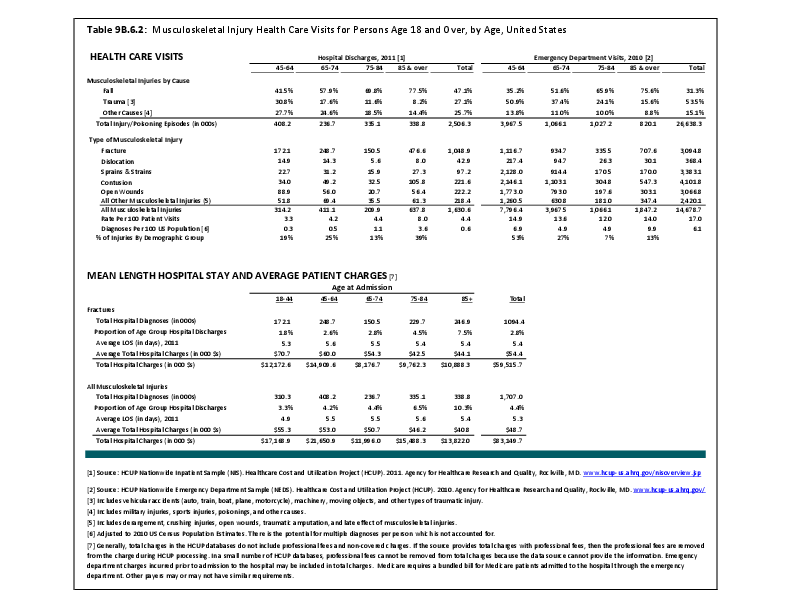
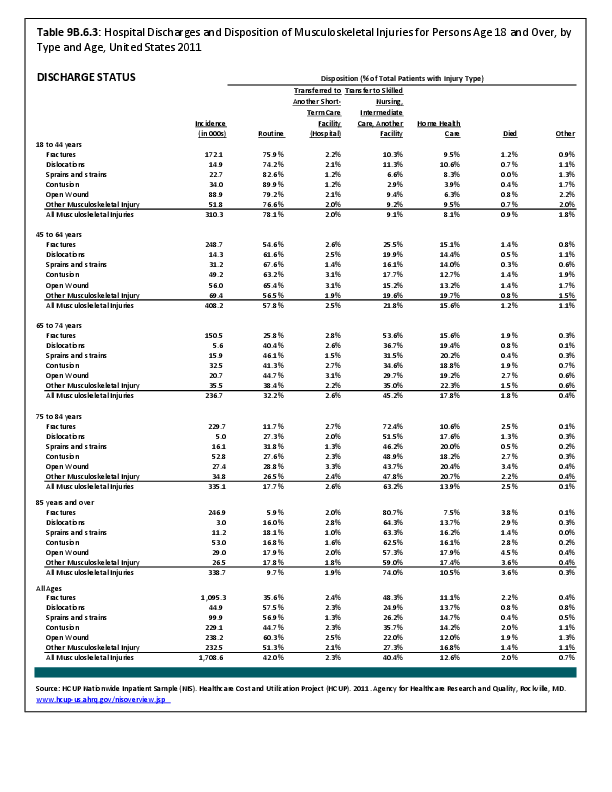
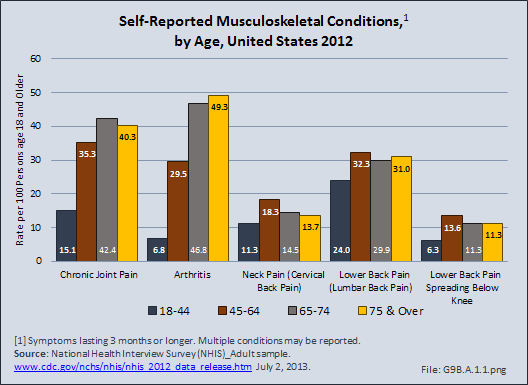
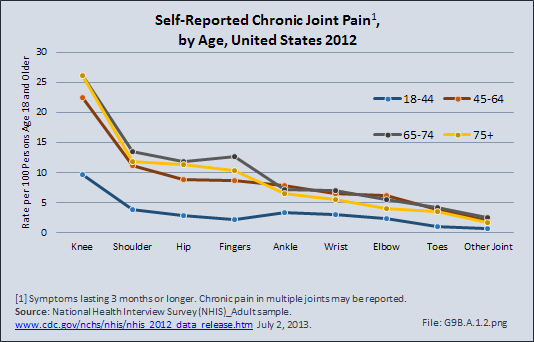
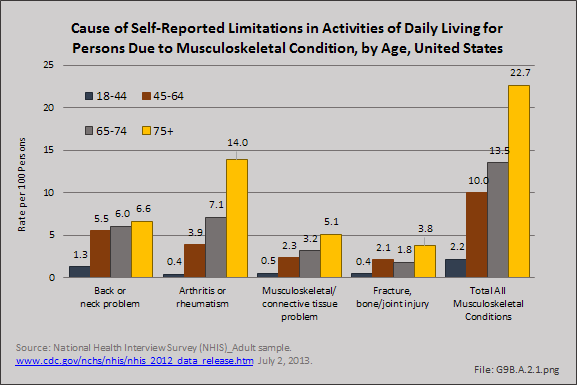
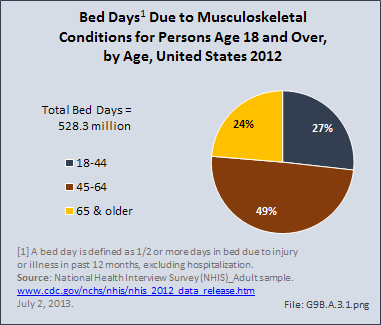
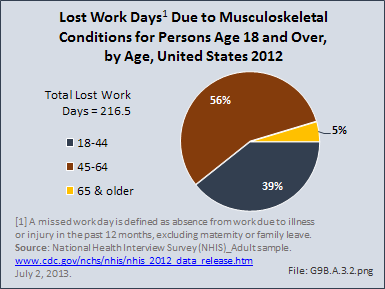
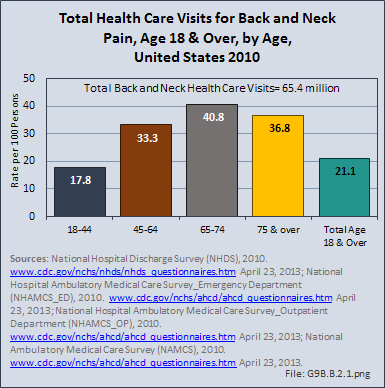
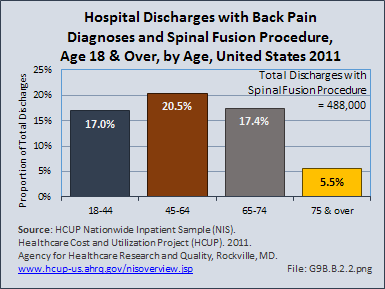
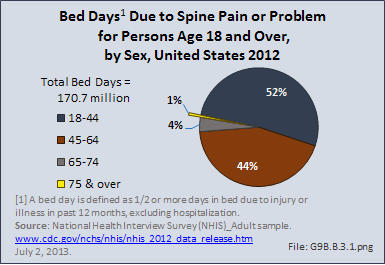
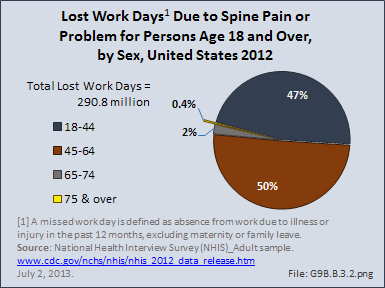
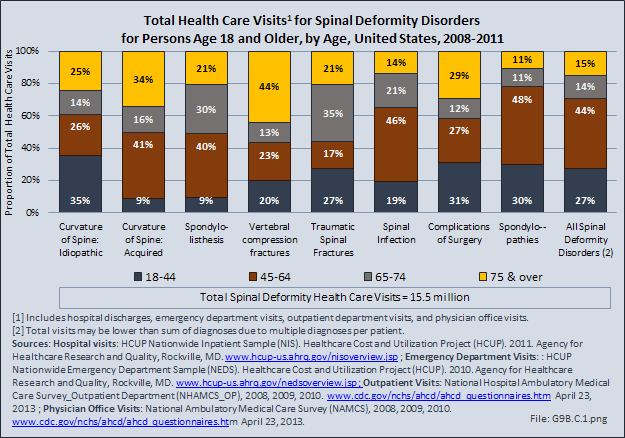
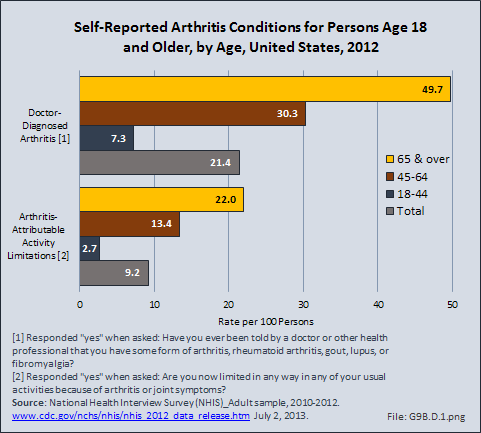
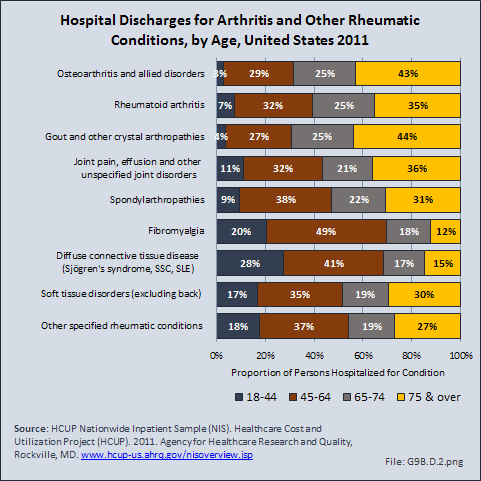
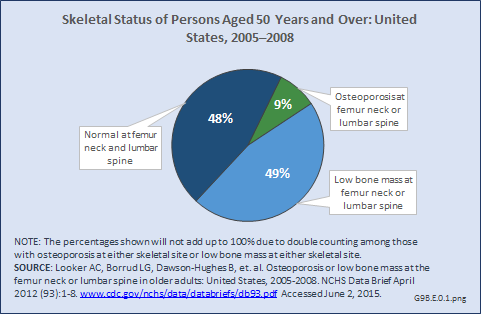
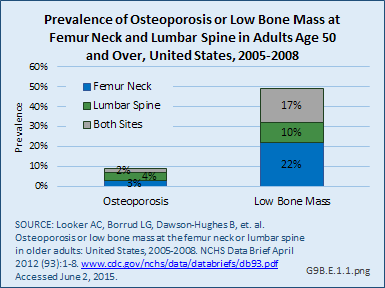
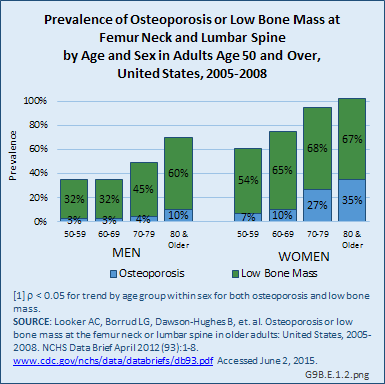
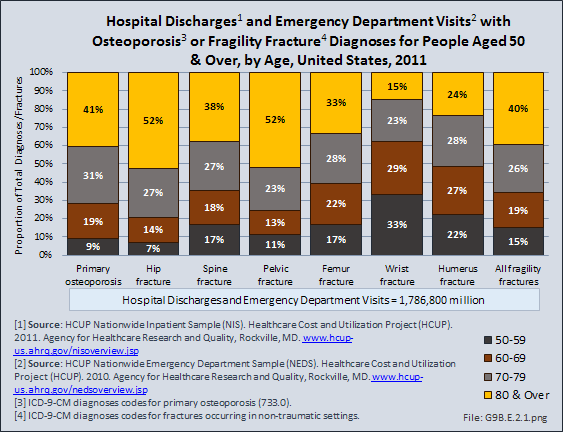
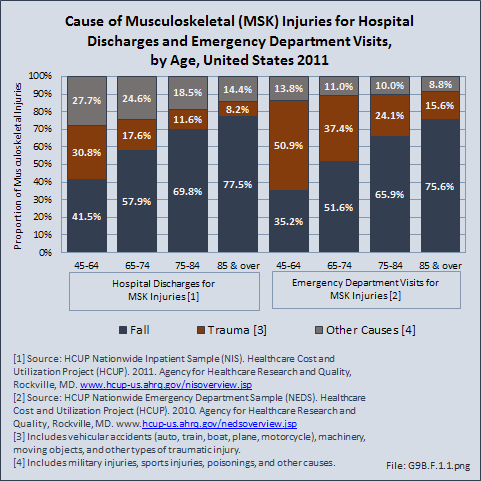
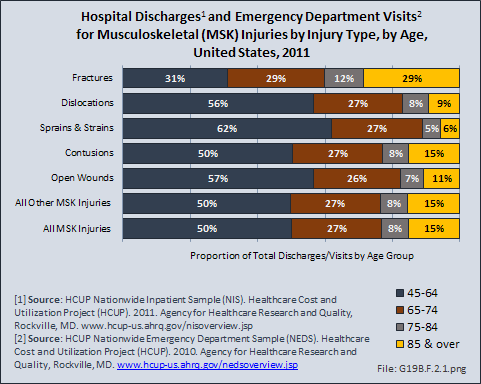
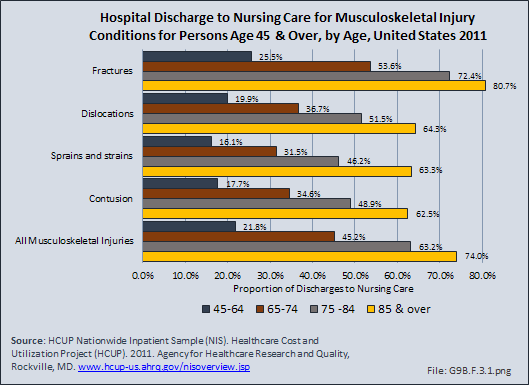
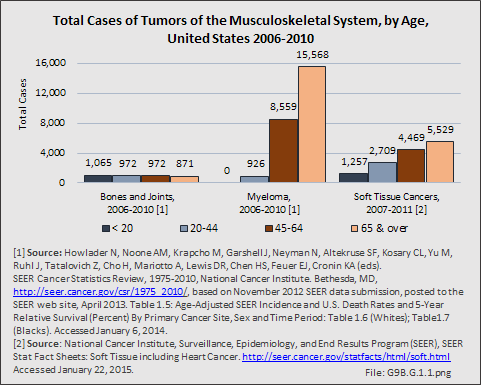
As expected, the aging population is prone to higher rates of nearly all musculoskeletal conditions than those found in younger people. In large part, these conditions can be attributed to wear and tear on bones and joints over a lifetime. However, some musculoskeletal conditions such as back pain are equally prominent in younger age populations, particularly those in their middle ages.
- 1. National Institute of Aging: NIH Seeking Strategies For Multiple Chronic Conditions In Older People. http://www.nia.nih.gov/newsroom/features/nih-seeking-strategies-multiple-chronic-conditions-older-people. Accessed March 2, 2015.
Edition:
- 2014

 Download as CSV
Download as CSV