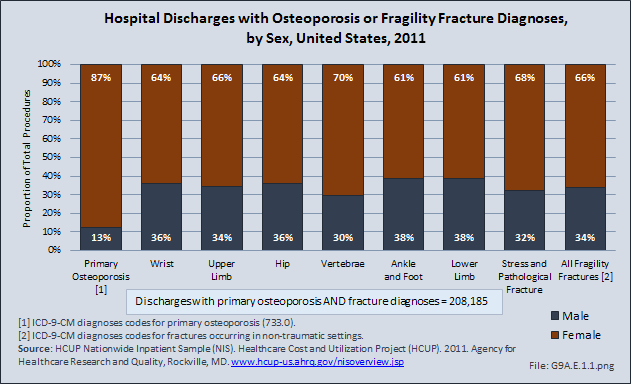
Osteoporosis was traditionally thought of as a condition affecting only women. Although approximately 80% of patients with the condition are female, it is being increasingly diagnosed among men. This increased incidence may reflect a greater awareness of the condition among men, rather than a true increase in incidence.
There are significant sex-based differences in osteoporosis. Osteoporosis in men tends to occur at an older age, unless another health condition intervenes. Osteoporosis in women is more likely primary and a result of estrogen loss, while osteoporosis in men is more likely to be secondary to another health condition, especially alcohol over-consumption, loss of testosterone, and use of corticosteroids.
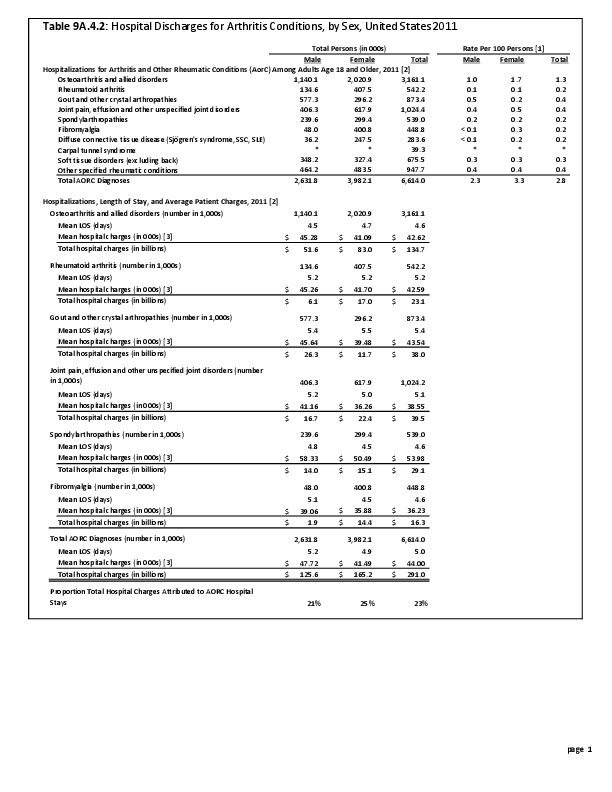
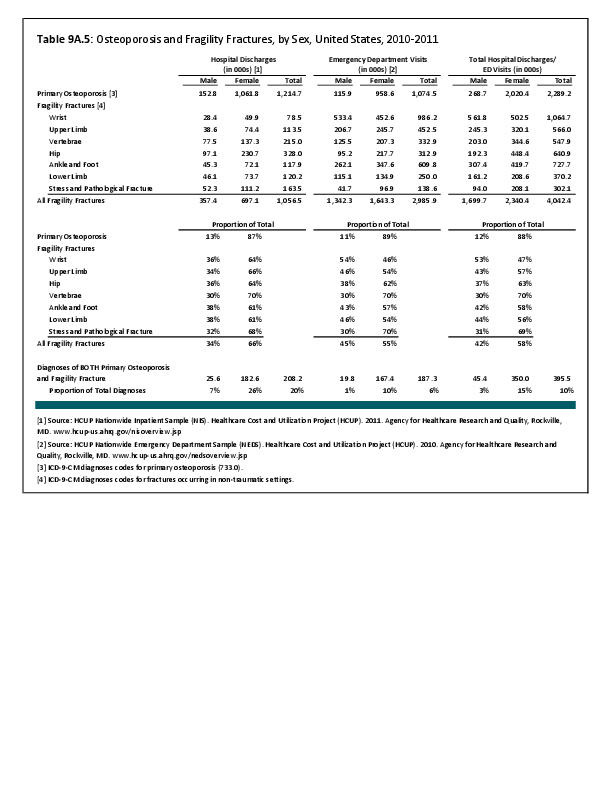
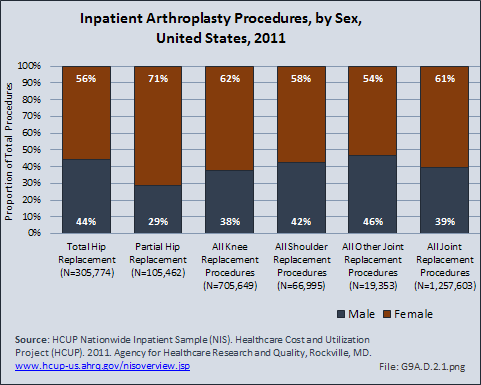
Low impact, or fragility, fractures, frequently occurring as the result of a simple fall, are more common among women, reflecting the higher incidence of osteopenia or osteoporosis. In 2011, 71% of partial hip replacements, most commonly performed to treat hip fractures, were performed on women. (Reference Table 9A.4.2 PDF CSV) For both sexes, the initial fragility fracture is the most significant risk factor for additional fractures and represents an opportunity for secondary prevention. Unfortunately, the likelihood of evaluation and attempts at secondary prevention measures are low for both sexes. However, men, more than women, are even less likely to be evaluated and treated for osteoporosis after the initial fragility fracture.1
For both men and women, low-impact fractures related to poor bone health have significant impact on function, morbidity, and mortality. Vertebral fractures, the most common fracture related to low bone mass, can lead to chronic pain, reduced subjective health status, and limitation in activities. The incidence of vertebral fractures increases with age for both sexes, although this is more pronounced among women.2 After adjusting for age and bone mineral density, sex-based risk for sustaining a vertebral fracture tends to be no longer significant.1 Smoking, alcohol consumption, and physical activity are known to impact bone health. However, studies examining their association with the risk of vertebral fractures have provided inconclusive evidence of sex-based differences in degrees of impact.3 The rate of mortality also is increased among those sustaining a vertebral fracture. However, Hasserius et al noted that the pattern of differences in mortality differed by sex: increased mortality in women was noted during the first decade after the fracture, especially the first 5 years; the greatest divergence in mortality among men was most significant during the first 3 years after the fracture.4 This is similar to the data available for outcome after fragility fractures of the hip. Hip fractures also lead to increased rates of disability and mortality; however, mortality is substantially higher among men sustaining a hip fracture, especially during the first year after the fracture. These differences in mortality after low-impact fracture, especially in the first few years after fracture, may reflect the differences in etiology of osteoporosis. Men, as previously noted, are more likely to have secondary osteoporosis and be older at the time of fracture; both of these most likely contribute to increased rates of mortality.
- 1. a. b. Rozental TD, Makhni EC, Day CS, Bouxsein ML: Improving evaluation and treatment for osteoporosis following distal radius fractures. JBJS (A) 2008;90(5):953-961.
- 2. Van Der Klift M, De Laet CEDH, Mccloskey EV, Hofman A, Pols HA: The incidence of vertebral fracture in men and women: The Rotterdam Study. J Bone Miner Res 2002;17:1051-1056.
- 3. Samelson EJ, Hannan MT, Zhang Y, et al. Incidence and risk factors for vertebral fracture in women and men: 25-year follow-up results from the population-based Framingham Study. J Bone Miner Res 2006;21(8):1207-1214.
- 4. Hasserius R, Karlsson MK, Jónsson B, et al: Long-term morbidity and mortality after a clinically diagnosed vertebral fracture in the elderly—a 12- and 22-year follow-up of 257 patients. Calcif Tissue Int 2005 Apr;76(4):235-242. Epub 2005 Apr 11.
Edition:
- 2014








 Download as CSV
Download as CSV