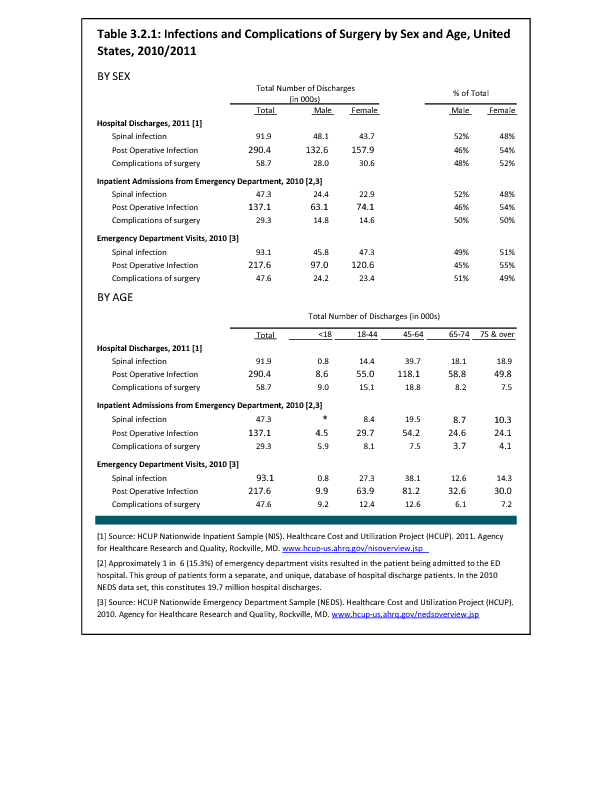
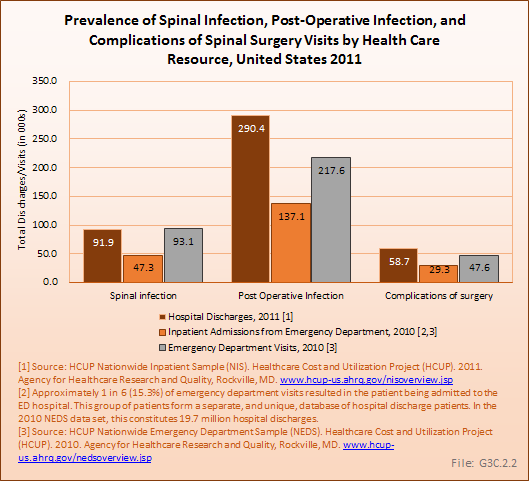
Spinal infections are usually the result of bacterial or fungal infections from other places in the body that spread to the spine though the bloodstream (hematogenously). Less commonly, they occur from local extension of a neighboring infection (eg, psoas abscess). Spinal infections are usually categorized by their location as discitis (infection of the vertebral disc space), vertebral osteomyelitis (infection of the vertebral body), and epidural abscess (infection of the spinal canal space). Vertebral osteomyelitis is the most common, with an estimated prevalence of 2.4 cases per 100,000 persons. The risk increases with age, and accounts for 4% to 6% of all cases of osteomyelitis. Epidural infections are relatively rare (0.2 to 1.2/10,000 hospital admissions), but are more likely to require emergent surgical treatment and are associated with significant morbidity and mortality rates.1,2,3
Postoperative wound infections and adverse events are relatively rare but are predictable risks and consequences of surgery. Although the absolute number is small in comparison to the volume of cases overall, they tend to have a disproportionate impact on both patient outcome and societal cost. There are many potential adverse events reported with any procedure, and the frequency and severity of these events varies based upon both patient and disease-specific variables. The codes included for query of the various databases for wound infections and adverse events are 996.2 (mechanical complication of nervous system device/implant), 996.59 (mechanical complication due to other implant/device), 996.63 (infection due to nervous system device/implant), 996.75 (other complications due to nervous system device/implant). Postoperative infections were queried for codes 998.51, 995.59, and 998.60. No differentiation was found in rates of infection between the spine and other areas within the body.
- 1. Zimmerli W: Vertebral osteomyelitis. N Engl J Med 2010;362:1022-1029.
- 2. Boeglin ER: Vertebral osteomyelitis presenting as lumbar dysfunction: A case study. JOSPT 1995;22(8):267-271.
- 3. Hlavin ML, Kaminski HJ, Ross JS, Ganz E: Spinal epidural abscess: A ten-year perspective. Neurosurgery 1990;27:177–84.
Edition:
- 2014











 Download as CSV
Download as CSV