There is a paucity of literature regarding racial differences in sports-related injuries. Anterior cruciate ligament rupture is a common sports injury. A retrospective study of women’s professional basketball players over a 4-year span reported a higher rate of ACL tears in white players than their African-American counterparts.1 A difference in femoral morphology has been found between racial groups and may be a contributor to the potential difference in ACL injury rates.2 Another significant sports injury, lower extremity tendon ruptures, was analyzed in a military database study. Quadriceps, patellar, and Achilles tendon ruptures were examined. African-American service members had a significantly higher rate of lower extremity tendon rupture when compared to white service members.3 A biomechanical study showed a higher Achilles tendon stiffness in black athletes which potentially makes them more susceptible to rupture.4
Ankle sprains are the most common injury in athletic populations.5 Both AA and white races have a higher rate of ankle sprains than Hispanics.6 This is potentially due to the difference in type of athletic activities, for example soccer vs basketball.
Falls are an important cause of hospital admission and can lead to injuries such as hip and distal radius fractures. Whites have a higher incidence of falls than African-Americans.7 In a prospective study, Kiely et al also found a higher rate of falls in whites; however, after adjusting for confounding variables including types of activity and community characteristics, the difference was minimized.8 According to a retrospective study by Strong et al, in patients 65 and older admitted for falls, AA patients have a higher risk of mortality after discharge from the hospital.9 This highlights the need for improved follow-up after discharge.
African-Americans have a lower overall incidence of fractures than whites.10,11; however, there is minimal research on fracture risk other than in the hip. Much of this is related to higher bone density in blacks along with the difference in activities engaged in. Some studies have also investigated for disparities in the management of fractures. Opel et al found that after adjusting for insurance status and severity of injury, African-Americans had significantly lower odds of receiving surgical treatment for humeral shaft fractures than white males.12 The results suggested a possible bias in treatment decision-making, leading to less aggressive management in African-Americans.
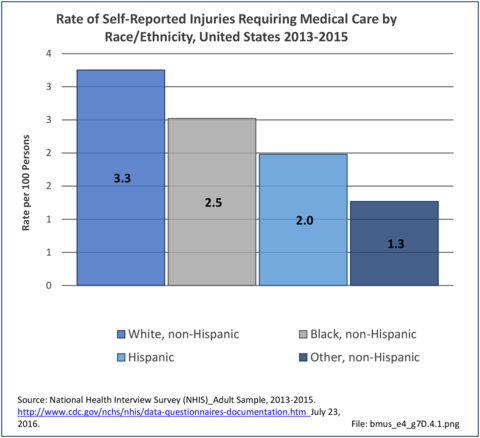
Self-Reported Injuries
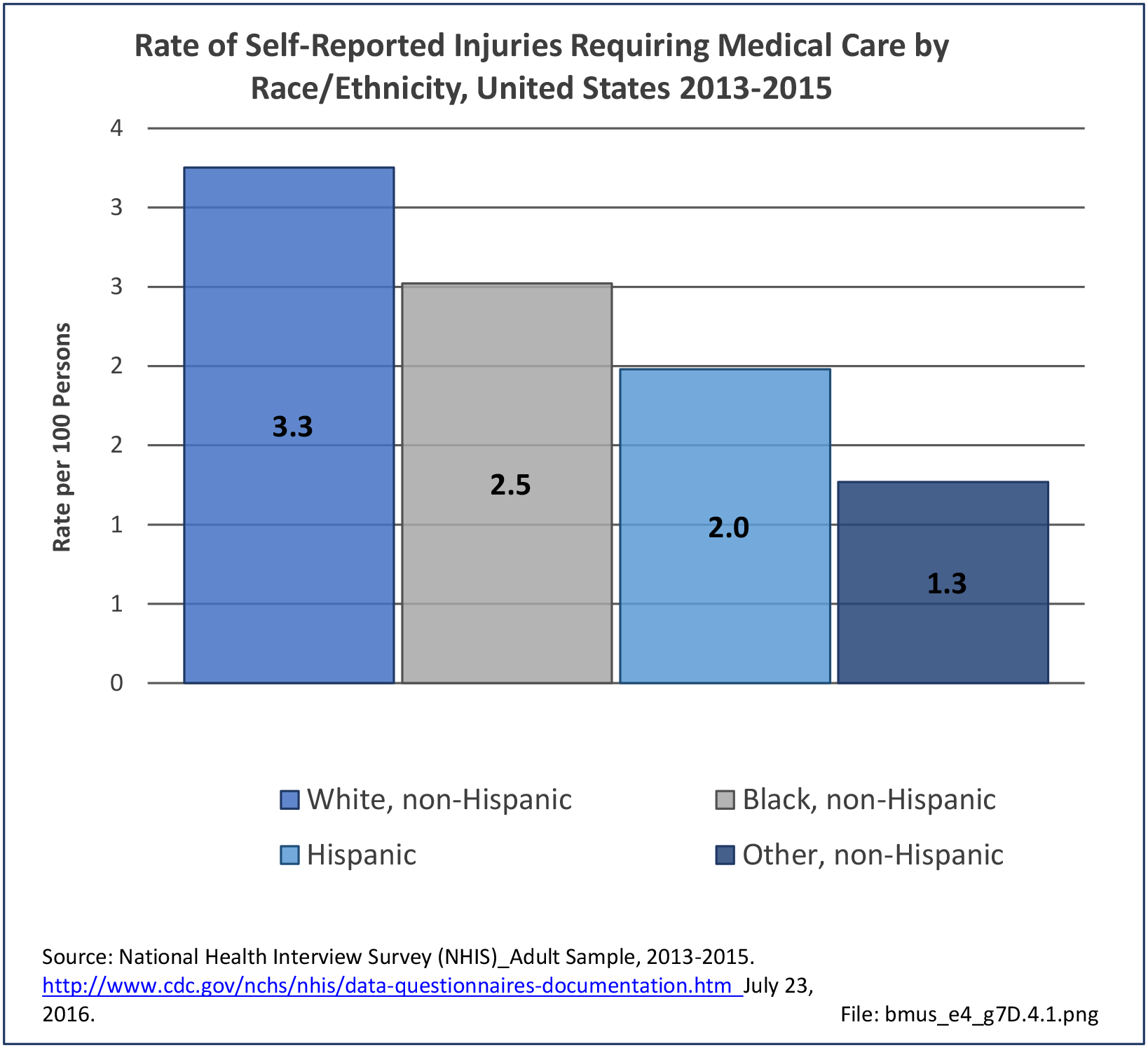
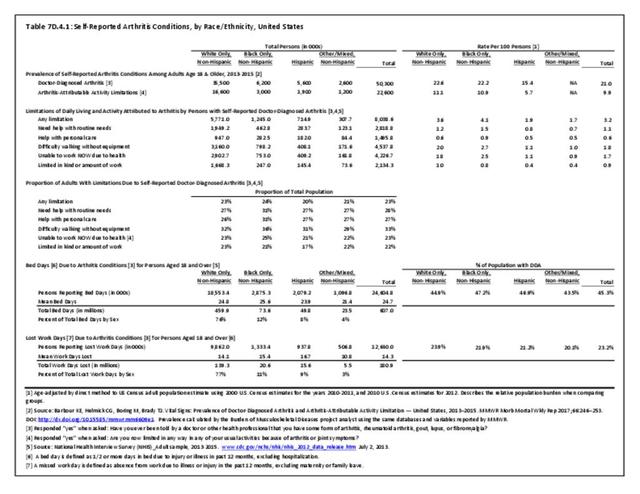
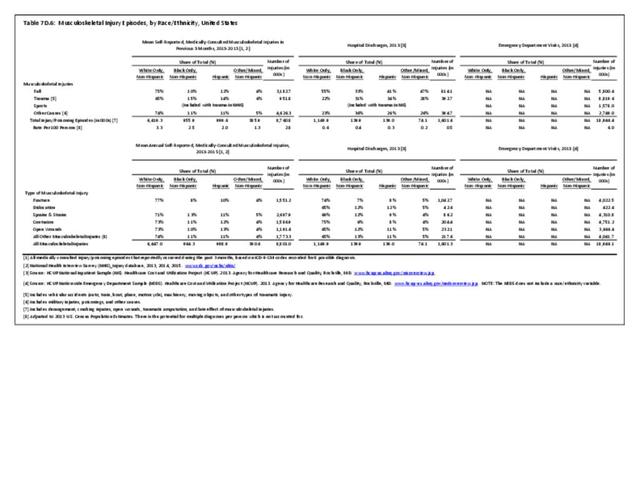
Non-Hispanic whites self-report the highest rate of injuries (3.3/100 persons) for which they sought medical care in 2013-2015. Non-Hispanic other/mixed race persons reported the lowest rate 1.3/100). (Reference Table 7D.6 PDF CSV)
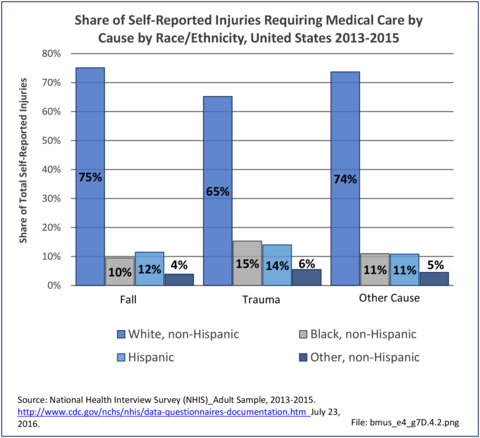
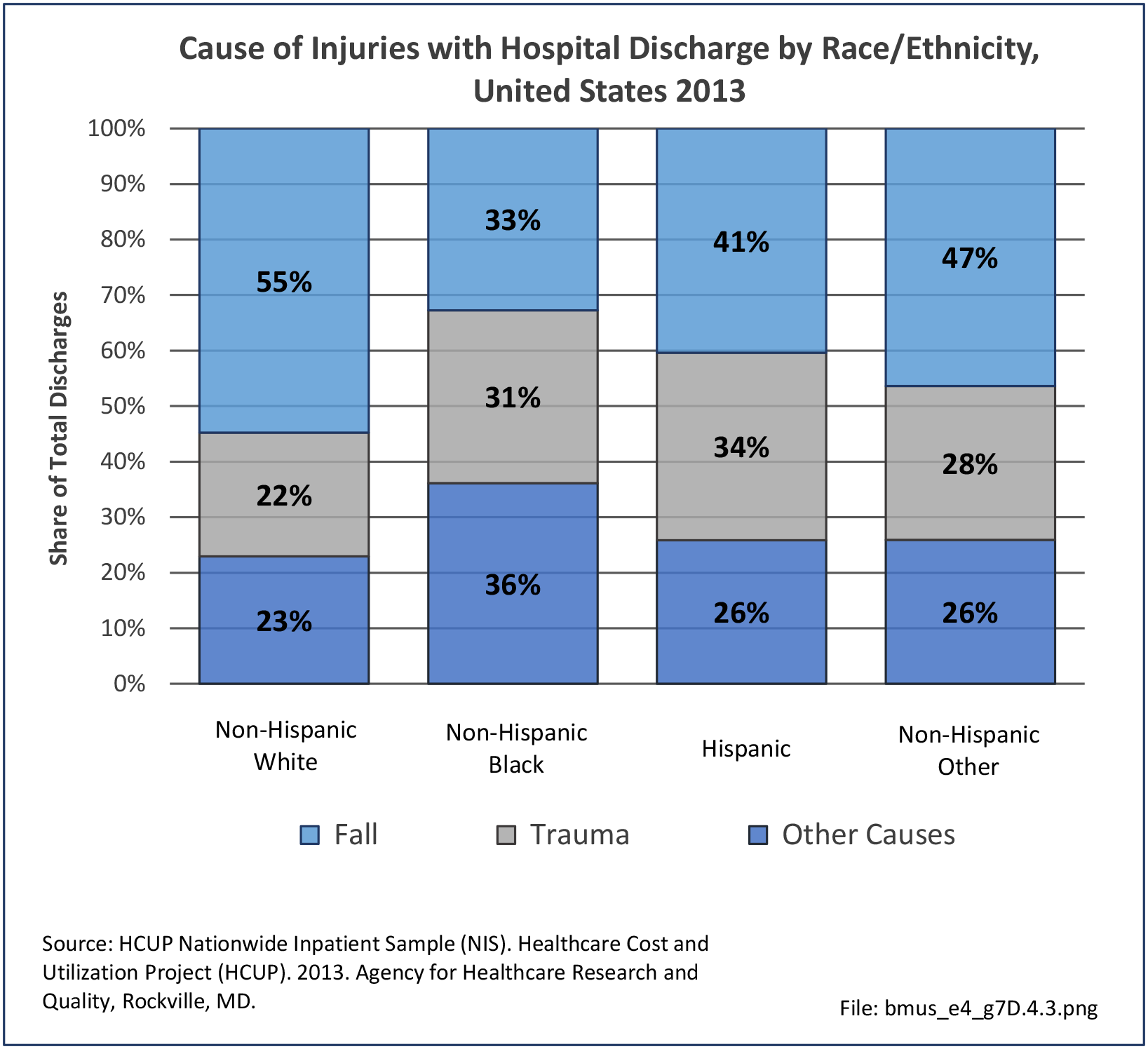
Cause of Injuries
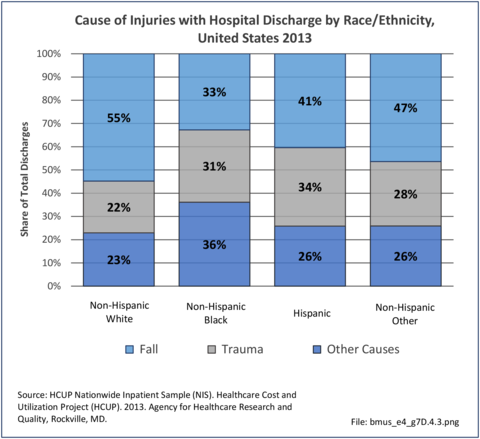
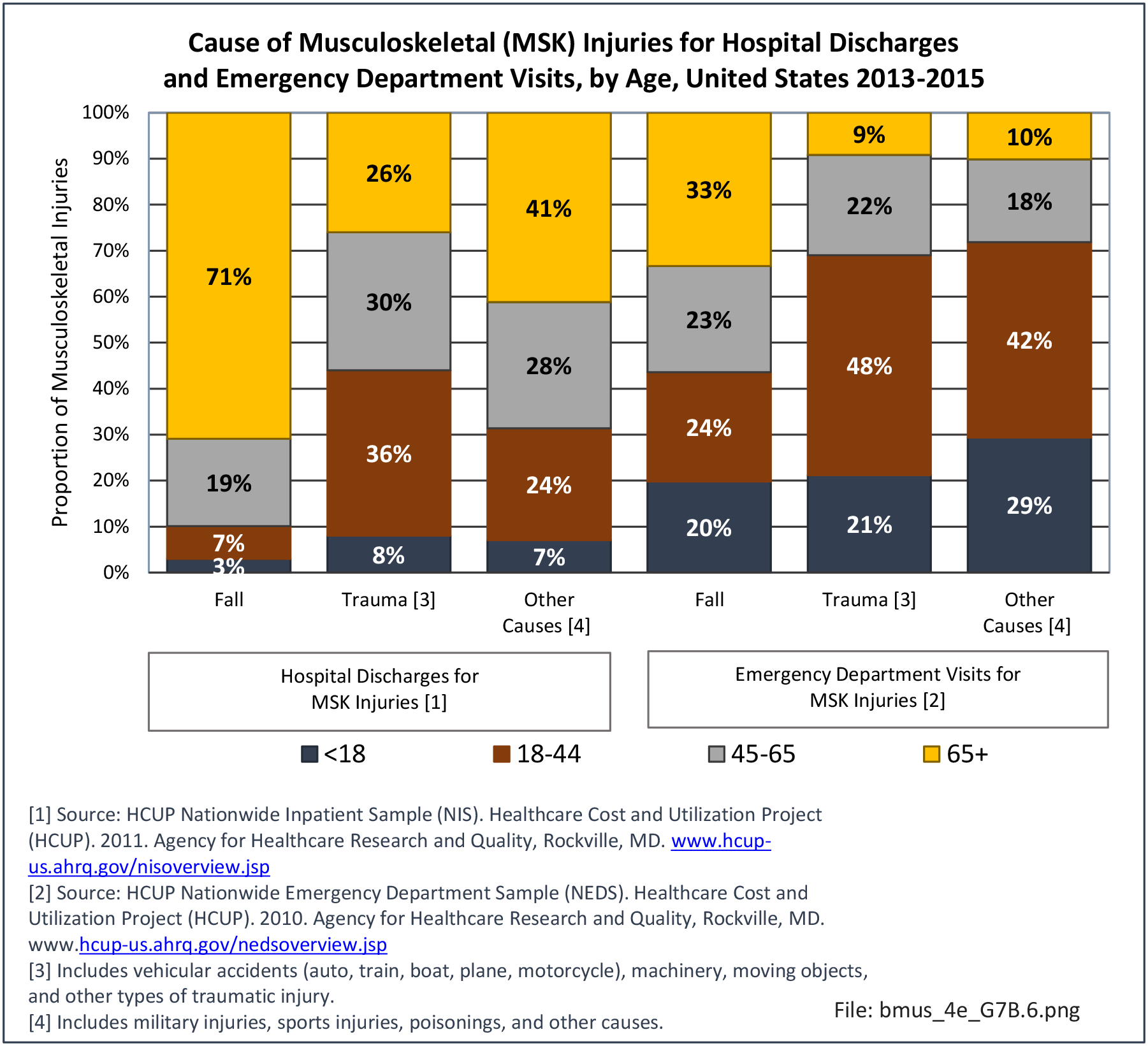
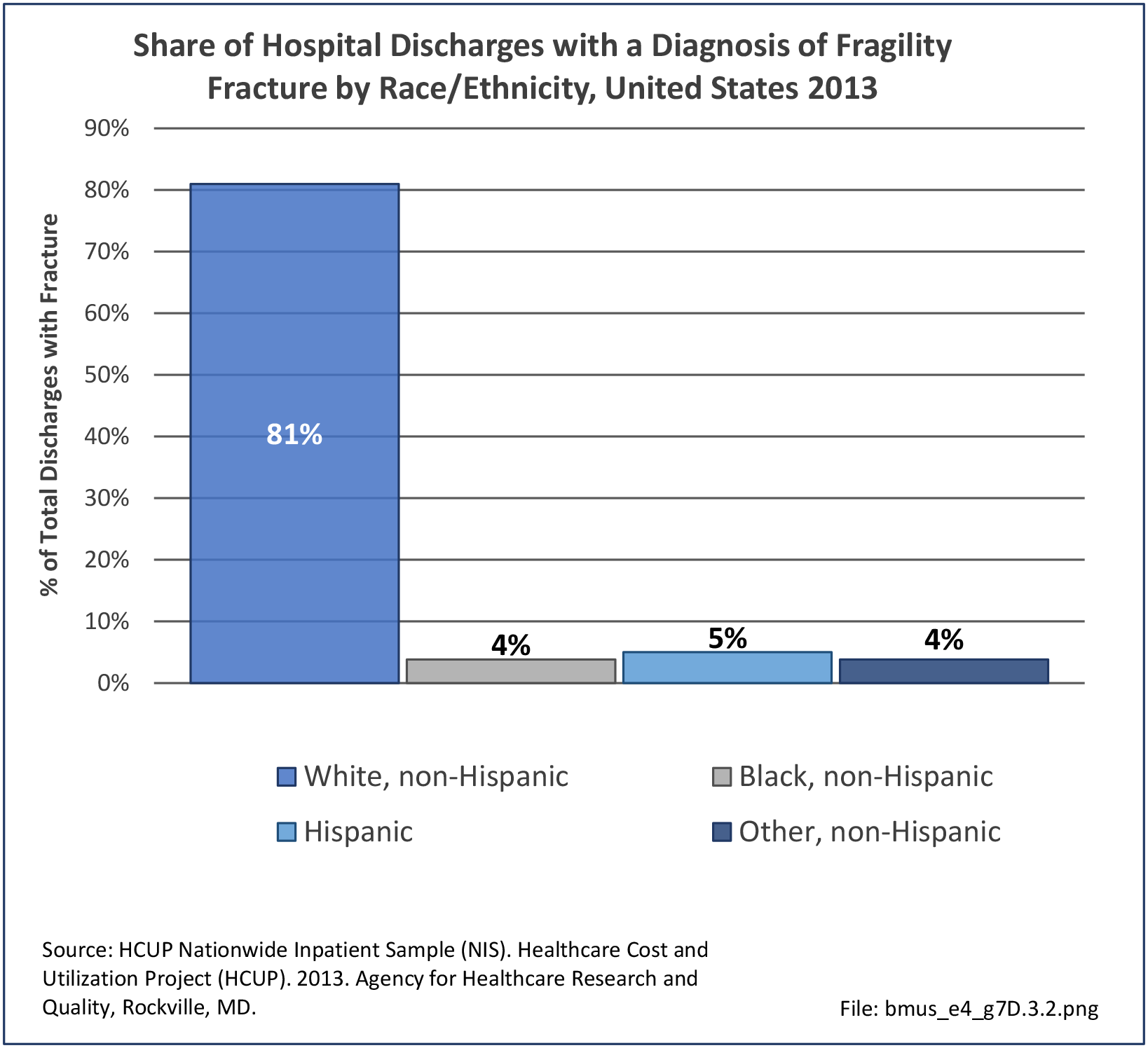
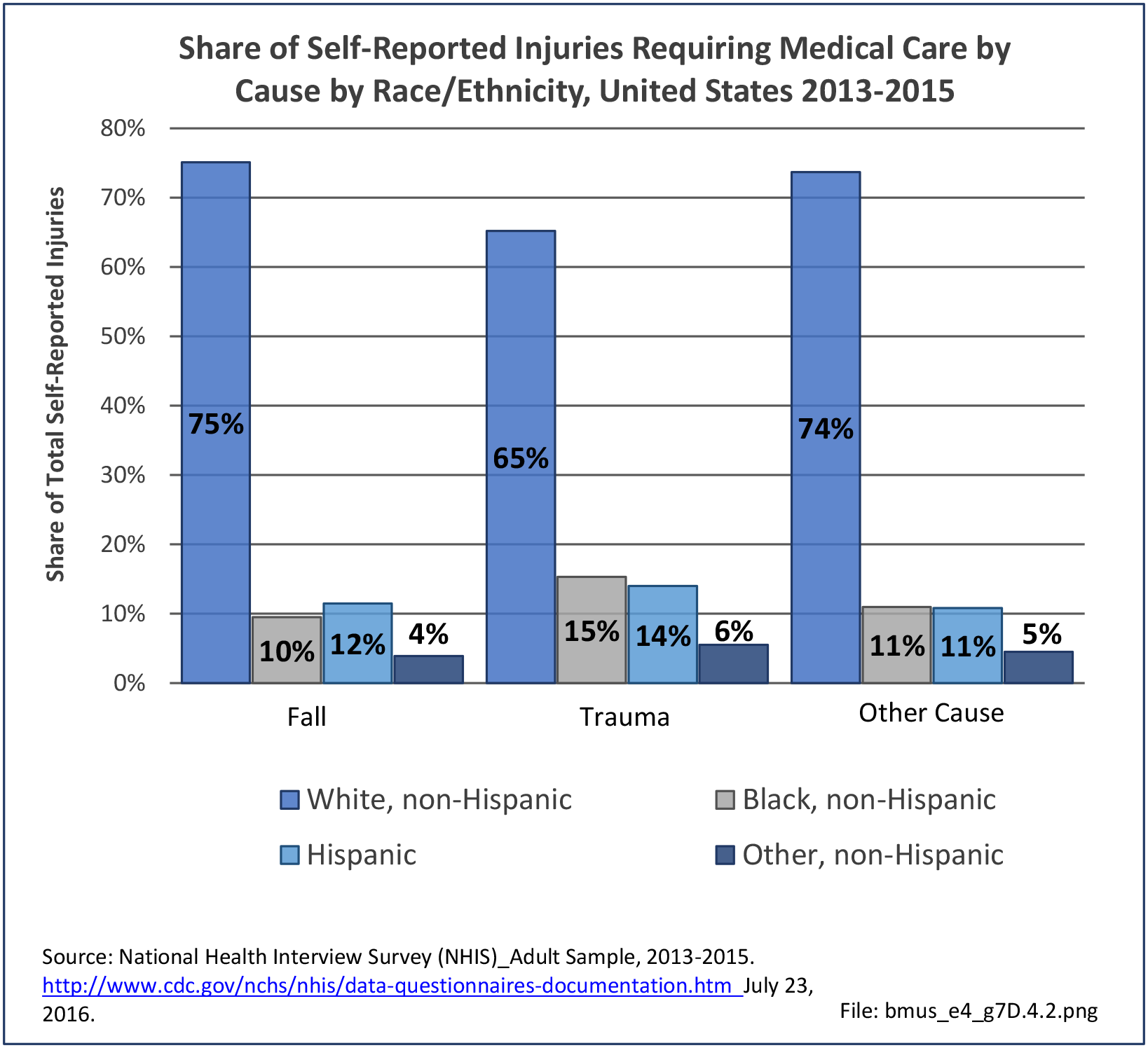
Data for both self-reported injuries for which medical care was sought and for hospital discharges support research findings reported above. Non-Hispanic white persons represented two-thirds or more of reported injuries from falls, trauma, or other causes, but were a smaller share of trauma accidents than falls or other causes.
Among hospital discharges for injuries, 55% of non-Hispanic white persons were hospitalized due to a fall, compared to 33% of non-Hispanic black persons. Persons of Hispanic ethnicity had the highest share of discharges due to trauma injuries (34%) , followed closely by non-Hispanic blacks (31%). (Reference Table 7D.6 PDF CSV)
- 1. Trojian TH, Collins S. The anterior cruciate ligament tear rate varies by race in professional women’s basketball. Am J Sports Med 2006;34(6):895–898.
- 2. Craig E. Intercondylar shelf angle: a new method to determine race from the distal femur. J Forensic Sci 1995;40(5):777-782.
- 3. Owens B, Mountcastle S, White D. Racial differences in tendon rupture incidence. Int J Sports Med 2007;28(7):617-620.
- 4. Fukashiro S, Abe T, Shibayama A, Brechue WF. Comparison of viscoelastic characteristics in triceps surae between Black and White athletes. Acta Physiol Scand 2002;175(3):183-187.
- 5. Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med 2007;37(1):73-94.
- 6. Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ Jr. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am 2010;92(13):2279-2284.
- 7. Geng Y, Lo JC, Brickner L, Gordon NP. Racial-ethnic differences in fall prevalence among older women: a cross-sectional survey study. BMC Geriatr 2017;17(1):65.
- 8. Kiely DK, Kim DH, Gross AL, et al. Fall risk is not black and white. J Health Dispar Res Pract 2015;8(3):72-84.
- 9. Strong BL, Torain JM, Greene CR, Smith GS. Outcomes of trauma admission for falls: influence of race and age on in hospital and post-discharge mortality. Am J Surg 2016;212(4):638-644.
- 10. Baron JA, Karagas M, Barrett J, et al. Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology 1996;7(6):612-618.
- 11. Griffin MR, Ray WA, Fought RL, Melton LJ 3rd. Black-white differences in fracture rates. Am J Epidemiol 1992;136(11):1378-1385.
- 12. Opel D, Rapone B, Krishnamoorthy B, Yoo J, Meeker J. Race and gender influence management of humerus shaft fractures. J Orthop 2018;15(2):540-544.
Edition:
- Fourth Edition