Recent emphasis has been placed on sagittal plane balance and restoring normal sagittal alignment with regards to the three dimensional deformity of adult spinal deformity (ASD), and is a primary condition leading to the high prevalence (68%) of persons age 60 and over with adult spinal deformity.1,2 The impact of sagittal plane alignment on the treatment of spinal disorders is of critical importance. A failure to recognize malalignment in this plane can have significant consequences for the patient not only for pain and deformity, but also social interaction due to deficient forward gaze. A good understanding of the principles of sagittal balance is vital to achieve optimum outcomes when treating spinal disorders. Even when addressing problems in the coronal plane (front from back), an awareness of sagittal balance is necessary to avoid future complications.3
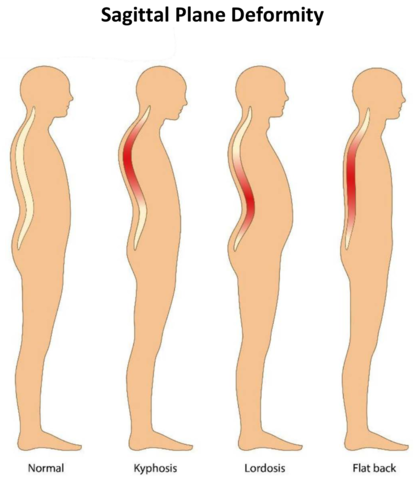
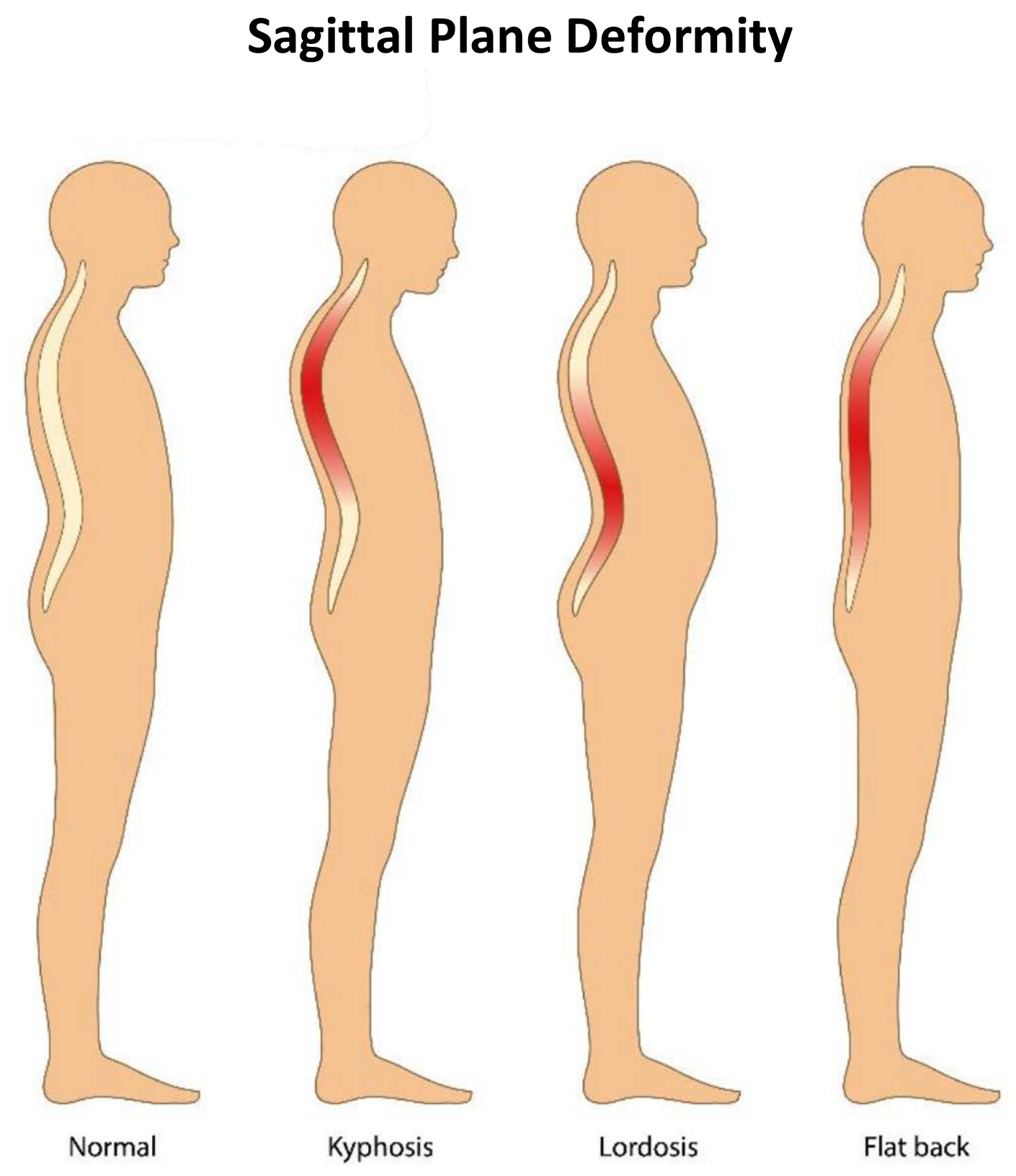
Sagittal plane deformity presents as an exaggeration or deficiency of normal lumbar lordosis (inward curving of the lumbar spine just above the buttocks) or kyphosis (exaggerated curvature of the upper (thoracic) spine). There are variations on the degree of normal curvature, still this shape allows equal distribution of forces across the spinal column. It is the disruption of this equilibrium by pathological processes or, as in most cases, ageing that results in deformity. This leads to adaptive changes in the pelvis and lower limbs. The effects of limb alignment on spinal posture are well documented. Changes in pelvic posture also affect spinal alignment.3
A lordosis deformity is usually iatrogenic (illness or condition caused by medication or treatment), and often follows lumbar fusion, thoracolumbar fusion, and, in some cases, lumbar decompressive procedures. Nonsurgical causes include ankylosing spondylitis, degenerative changes, or adult presentation of adolescent idiopathic scoliosis. The deformity may lead to neurogenic radicular symptoms secondary to stenosis, paraspinal muscular fatigue, and low back pain. Nonoperative treatment options fail for most patients. Surgical interventions are aimed at restoring lumbar lordosis, which is typically accomplished with revision decompression, fusion, and various osteotomies.4
Kyphosis is often secondary to inflammatory, degenerative, or post- traumatic disorders, and can be caused by poor posture, slouching, osteoporosis, birth defects, or disease. They may also be secondary to infection or tumors. There is usually pain and functional disability along with concerns about self-image and social interaction due to inability to maintain a horizontal gaze. The resultant pelvic and lower limb posture is an attempt to restore normal alignment. Addressing this complex problem requires detailed expertise and awareness of the potential pitfalls surrounding its treatment.1
Increasingly positive sagittal imbalance has been shown to correlate with poor functional outcome and poor self-image along with poor psychological function. Restoring normal spinopelvic alignment is paramount to the treatment of complex spinal deformity with sagittal imbalance. Understanding of whole spinal alignment and dynamics of spinopelvic alignment is essential to restore sagittal balance while minimizing the risk of developing sagittal decompensation after surgical intervention.1,3
Management of Sagittal Deformity
The goal of sagittal deformity management is to maintain the body in an energy-efficient, ergonomically favorable erect position. The larger the deviation from a balanced alignment, the more energy an individual uses to stand upright without external suport. Patients with symptomatic sagittal plane deformity often present with a sagittal balance at the periphery of this balanced alignment, leading to an increased effort of accessory musculature to maintain the head over the pelvis. This leads to fatigue and pain, especially with prolonged activity. As sagittal imbalance progresses, different compensatory mechanisms such as the pelvic retroversion, hip extension, and knee flexion are used in order to restore and maintain sagittal balance. Once a spinal deformity surpasses these compensatory mechanisms surgical intervention is often requested.5
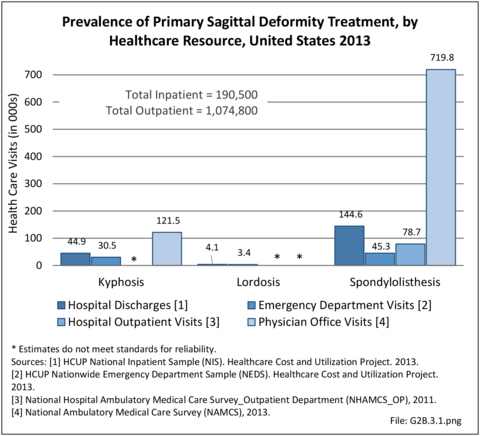
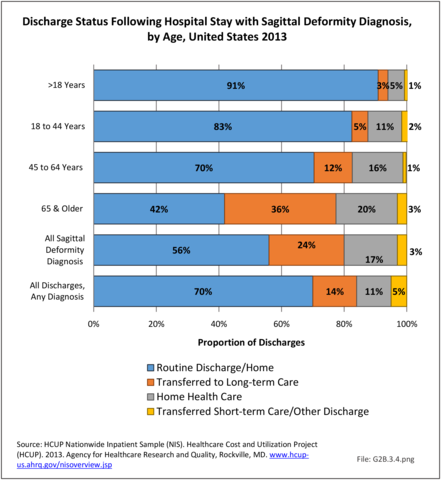
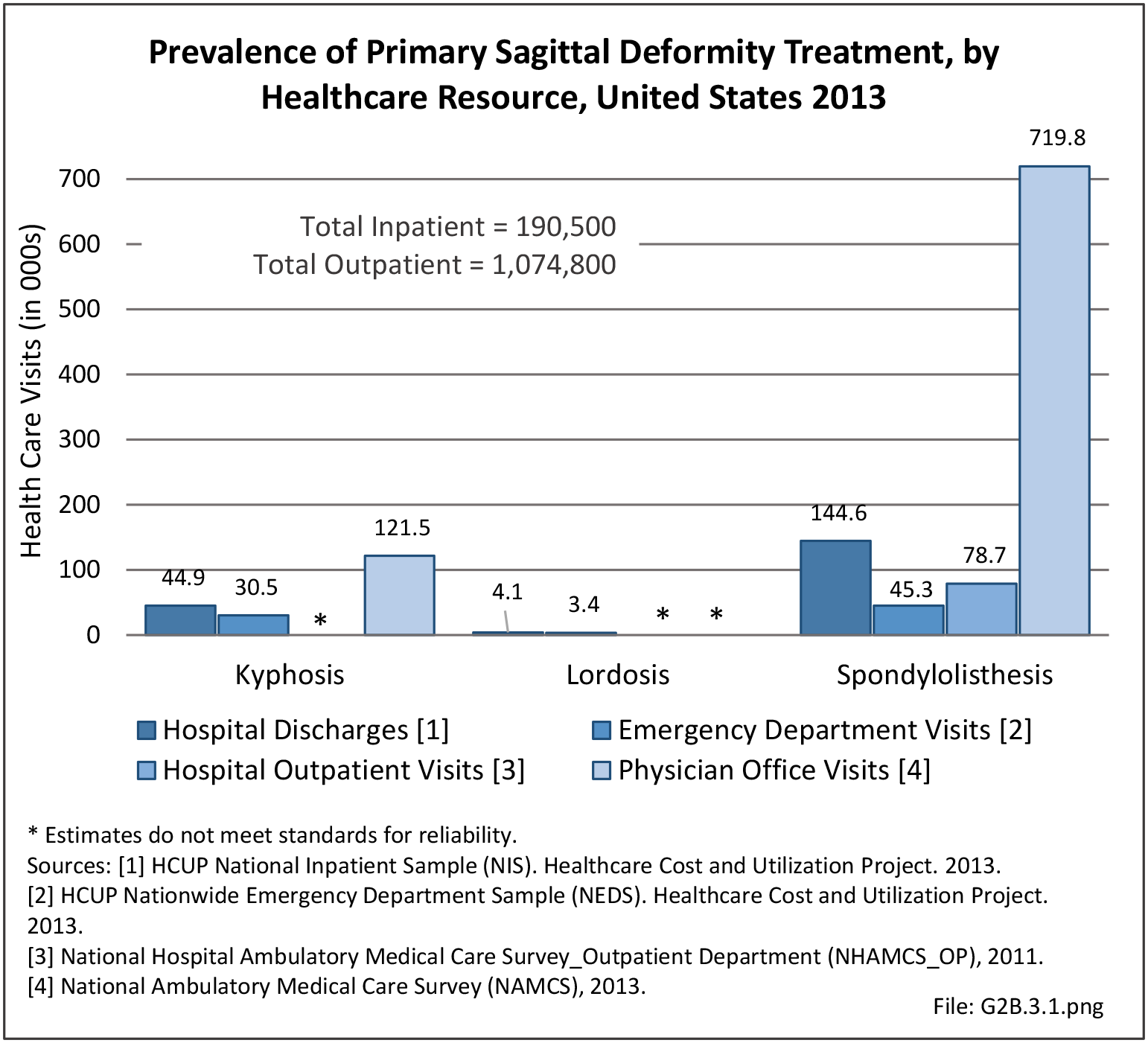
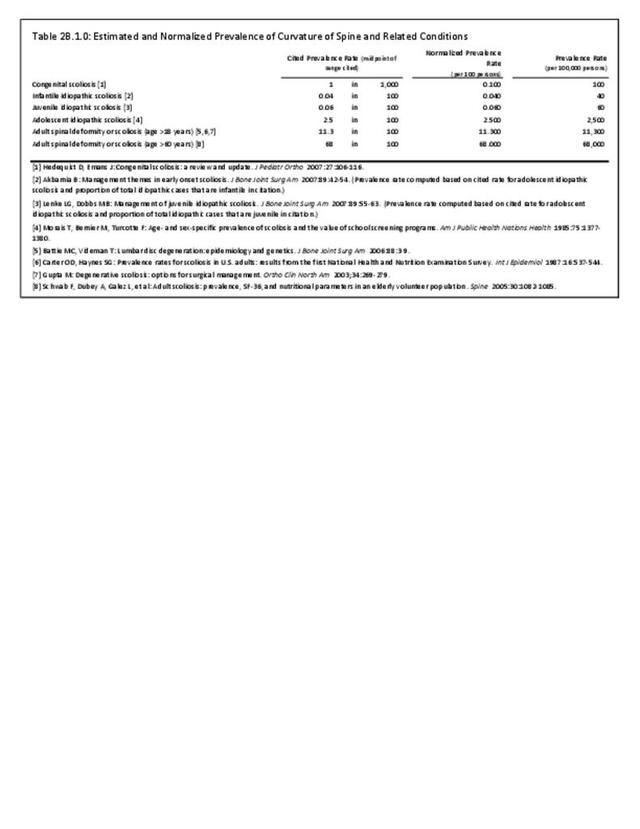
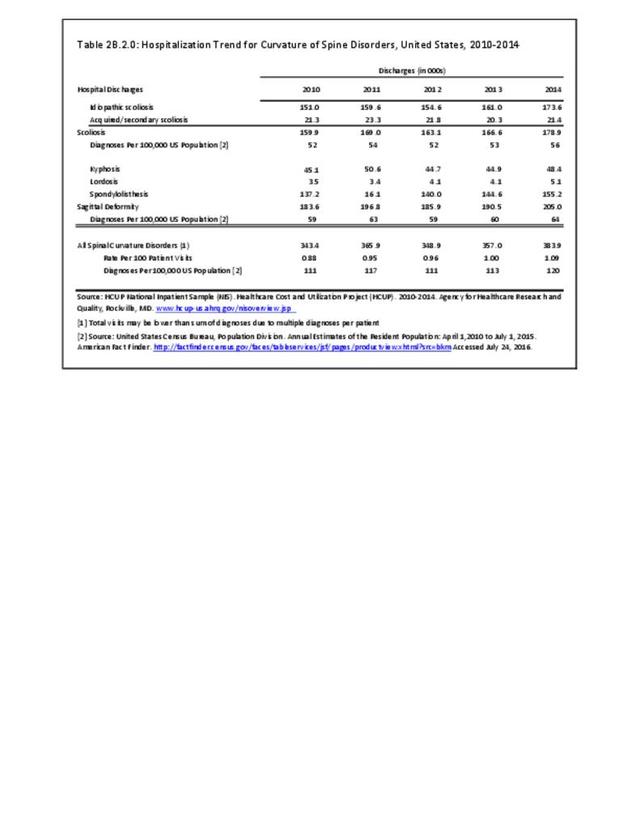
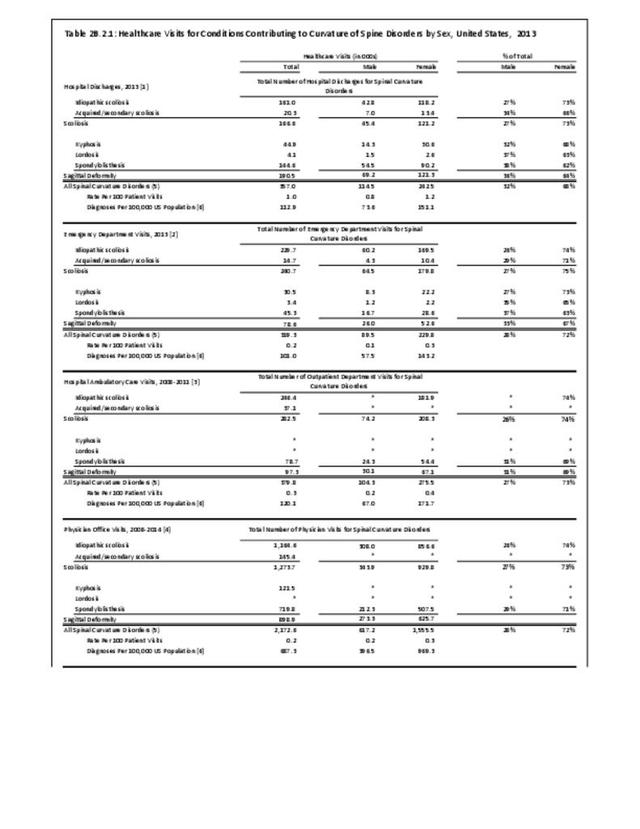
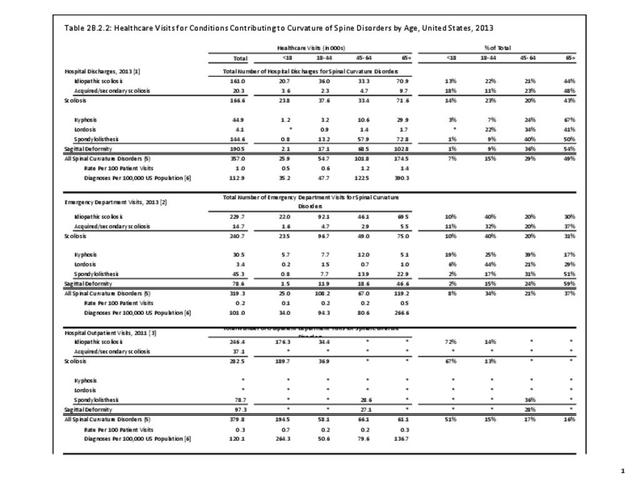
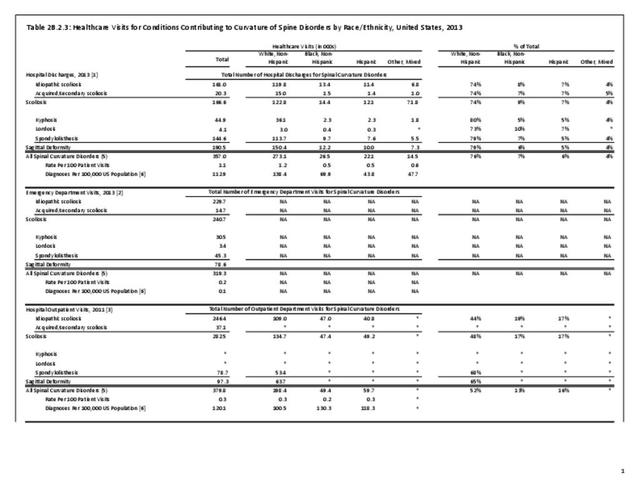
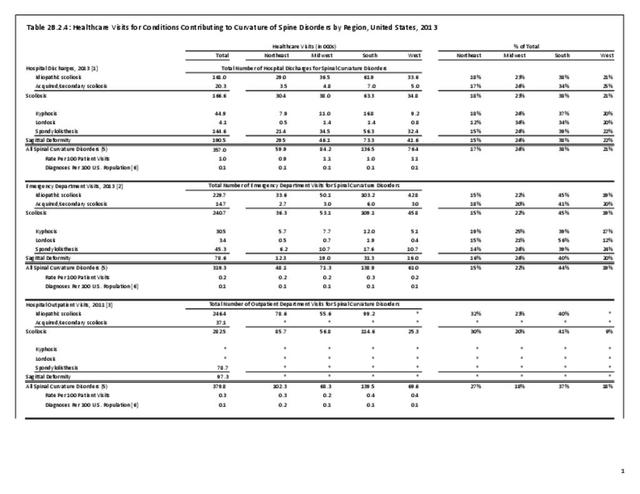
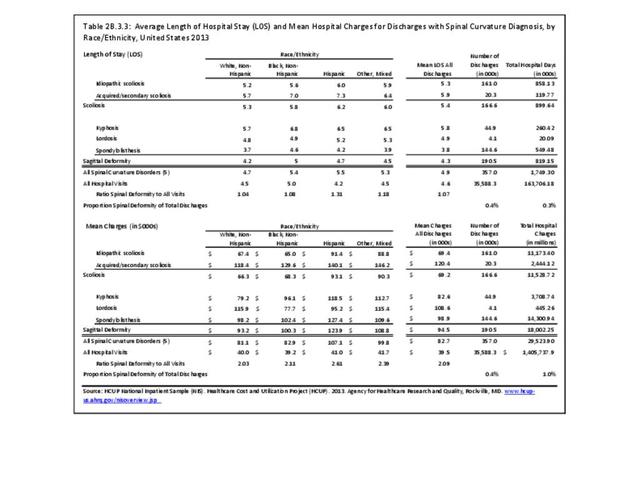
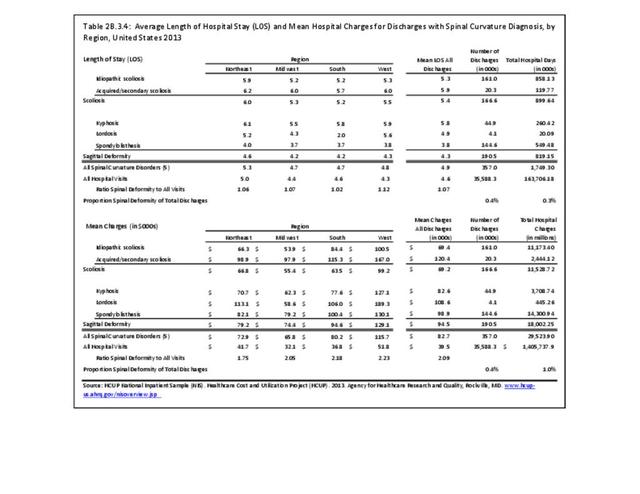
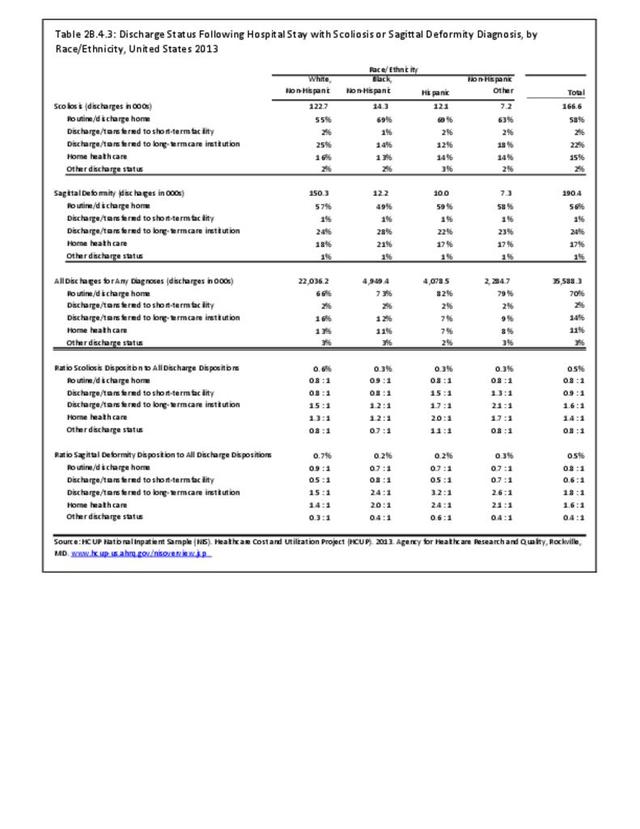
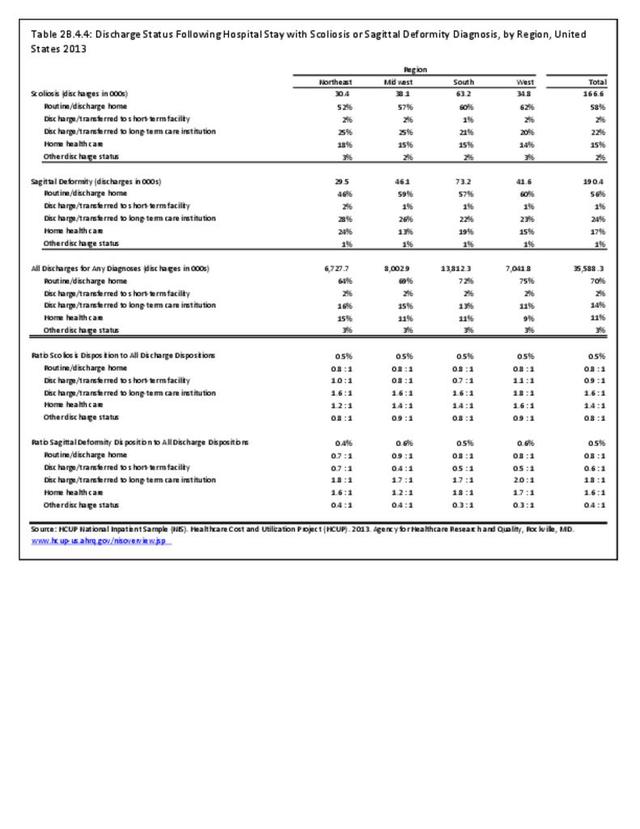
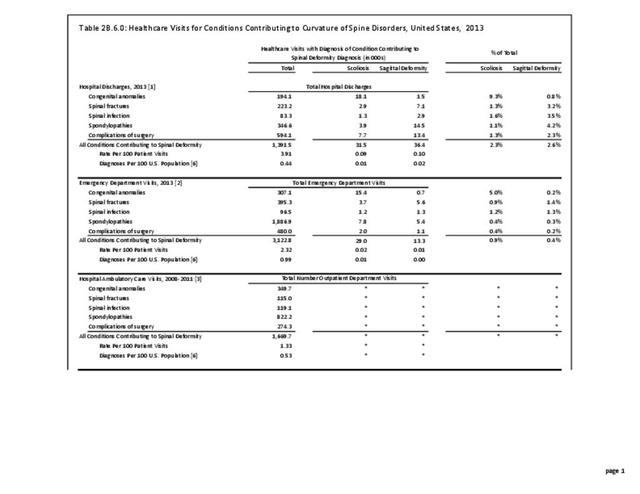
Operative management of sagittal deformity in the adult encompasses a spectrum of procedures with fusion the most common. In 2013, a query of the Healthcare Costs and Utilization Project (HCUP) Nationwide Inpatient Survey (NIS) resulted in approximately 190,500 hospitalizations associated with a discharge diagnosis of sagittal deformity. The largest share (76%), or 144,600 patients, were diagnosed with spondylolisthesis. Hospitalization with a sagittal deformity diagnosis was higher among the elderly, accounting for more than one-half (54%) among all ages for those 65 and older. Females accounted for 69% of all sagittal deformity hospitalizations. Race/ethnicity and region in the US did not show significant differences. (Reference Table 2B.2.1 PDF CSV, Table 2B.2.2 PDF CSV, Table 2B.2.3 PDF CSV, Table 2B.2.4 PDF CSV)
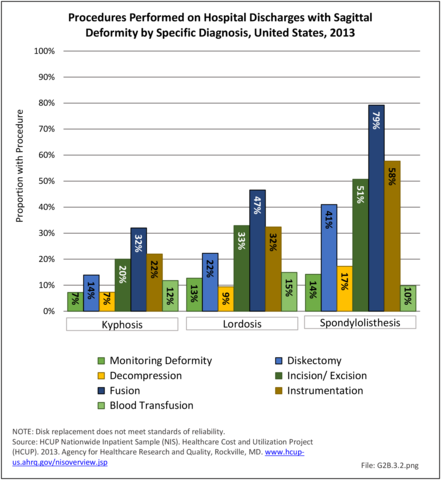
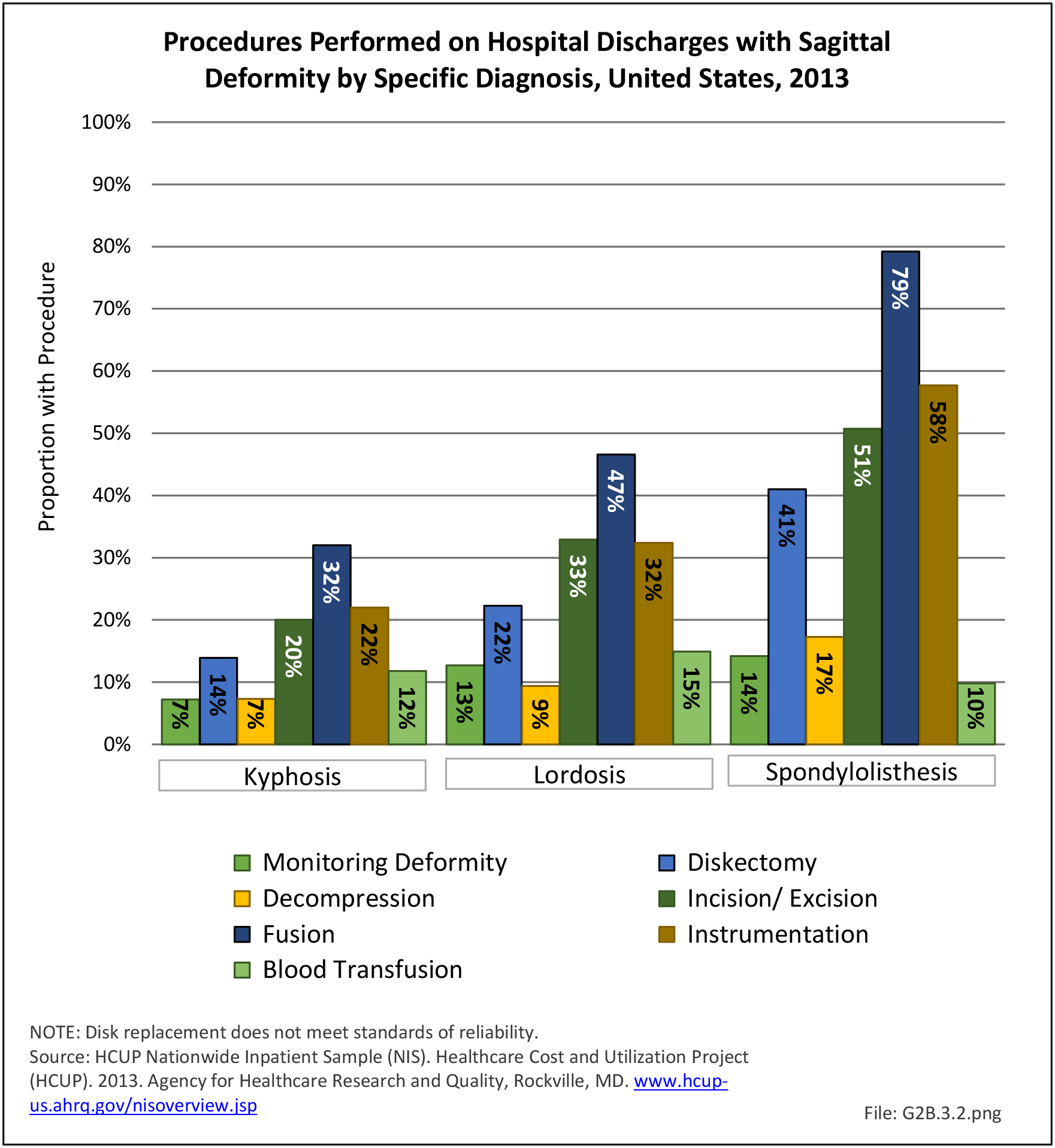
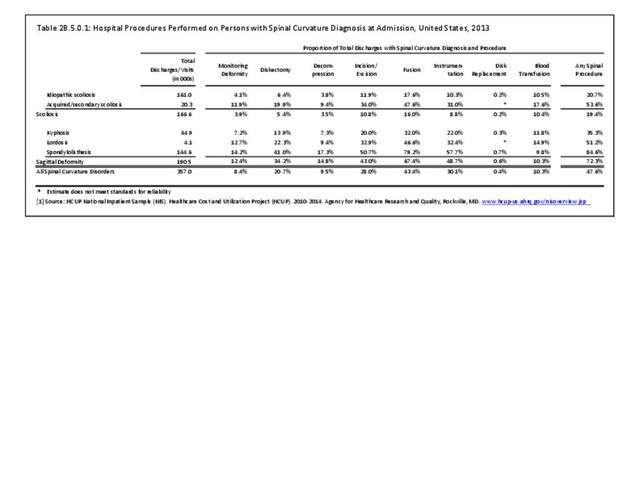
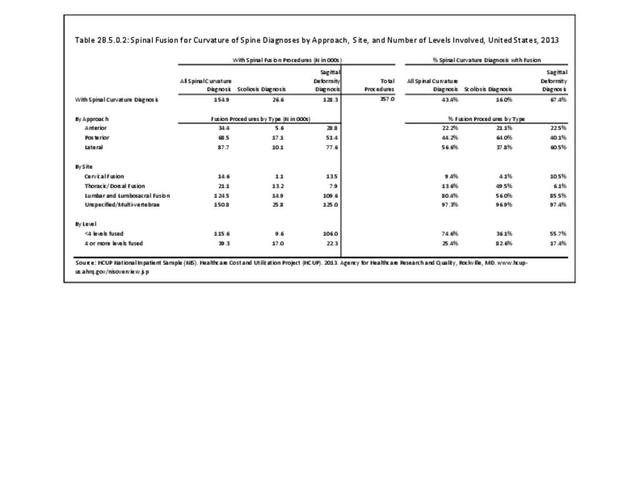
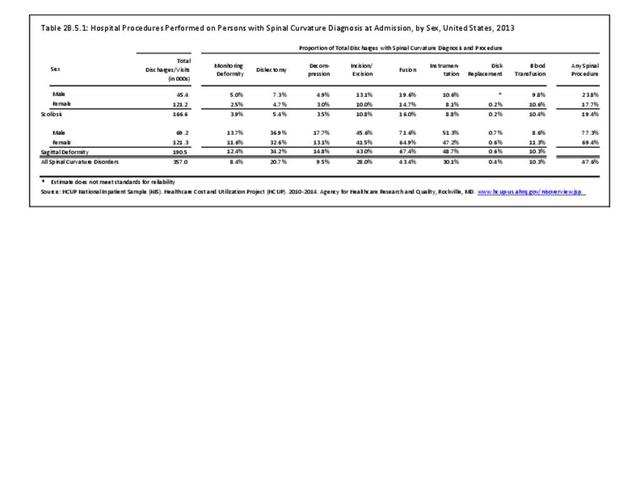
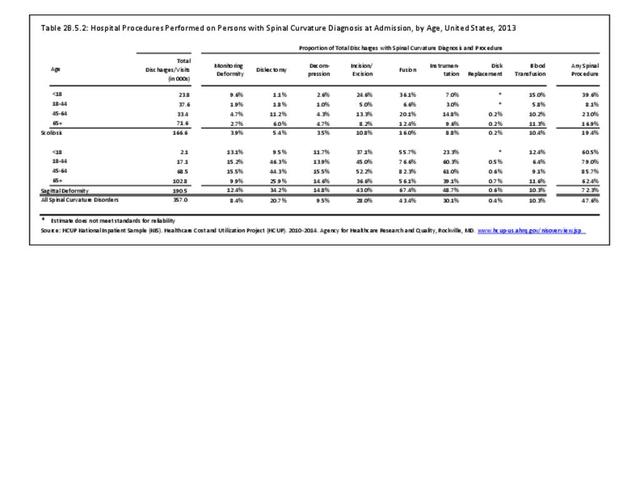
In 2013, more than nearly three-fourths (72.3%) of patients with a diagnosis of sagittal deformity had a surgical procedure. A diagnosis of spondylolisthesis had the highest rate (84.6%) of surgical procedure. The most common procedure performed on sagittal deformity patients was spinal fusion, with 67.4%, having this procedure. More than one-half (56%) had fusion of less than four levels. Sex of the patient was not a factor in having a procedure, but persons age 45 to 64 were most likely to have a procedure. (Reference Table 2B.5.0.1 PDF CSV, Table 2B.5.0.2 PDF CSV, Table 2B.5.1 PDF CSV, Table 2B.5.2 PDF CSV)
Sagittal balance is an independent predictor of clinical outcomes in spinal care. Surgical treatment is challenging and jeopardized by frequent complications. Guidelines for surgical treatment are currently not based on a classification of the disease. A comprehensive classification of sagittal balance based on regional deformities and compensatory mechanisms combined in deformity patterns is proposed. Though the sagittal shape of the spine can change due to degeneration or trauma, correlations between sagittal shape parameters and pelvic incidence (PI) have been described. PI is not changed by degeneration, thus representing a permanent source of information on the original sagittal shape of the spine.6
Burden of Sagittal Deformity
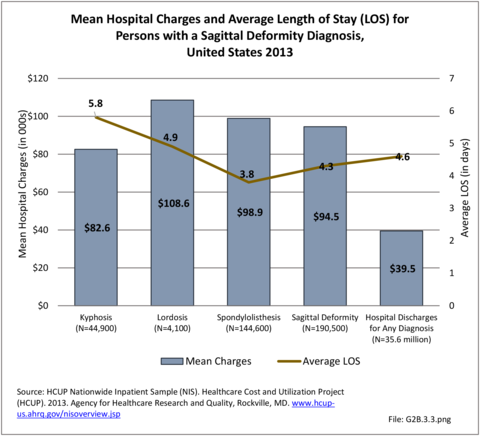
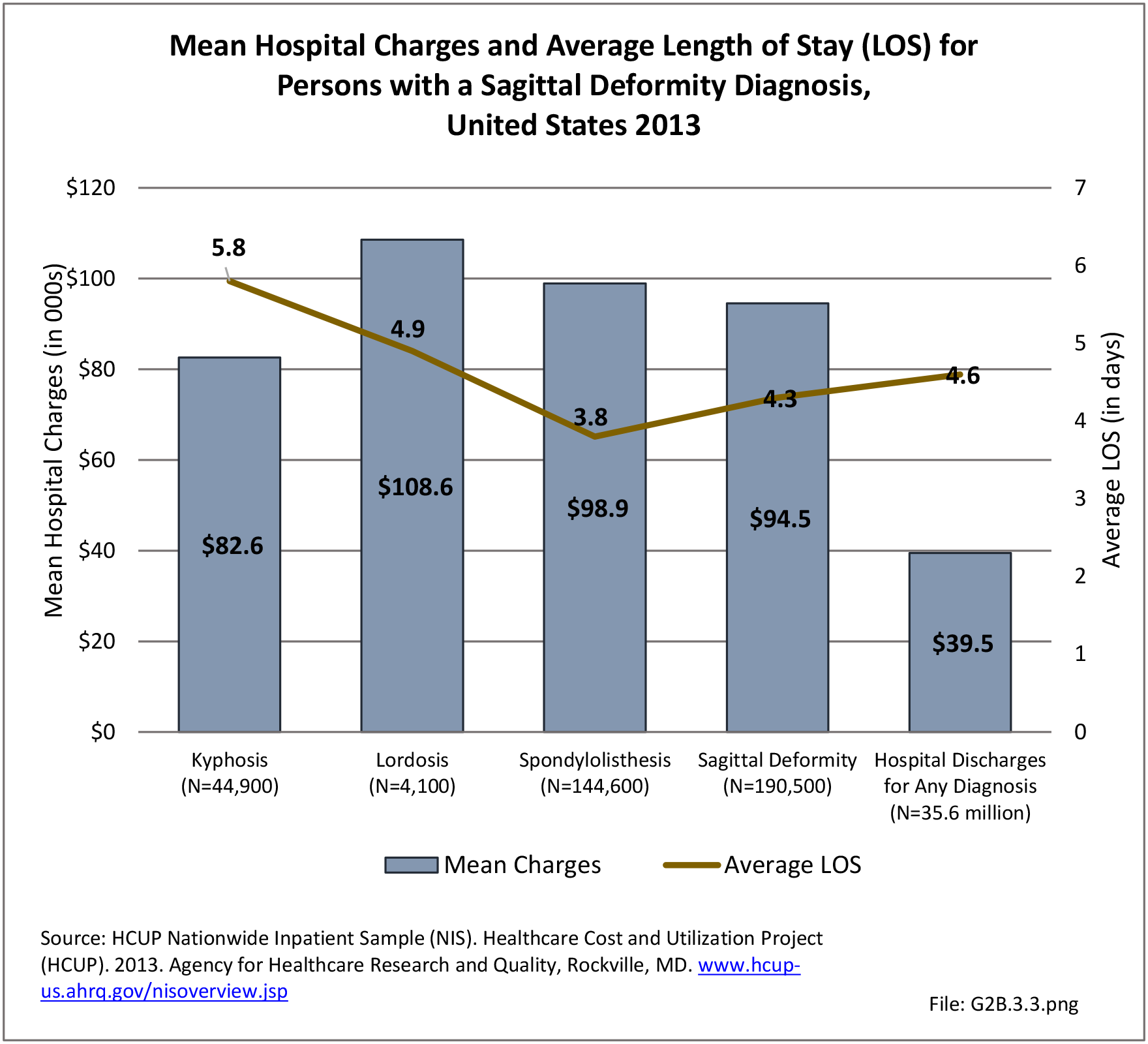
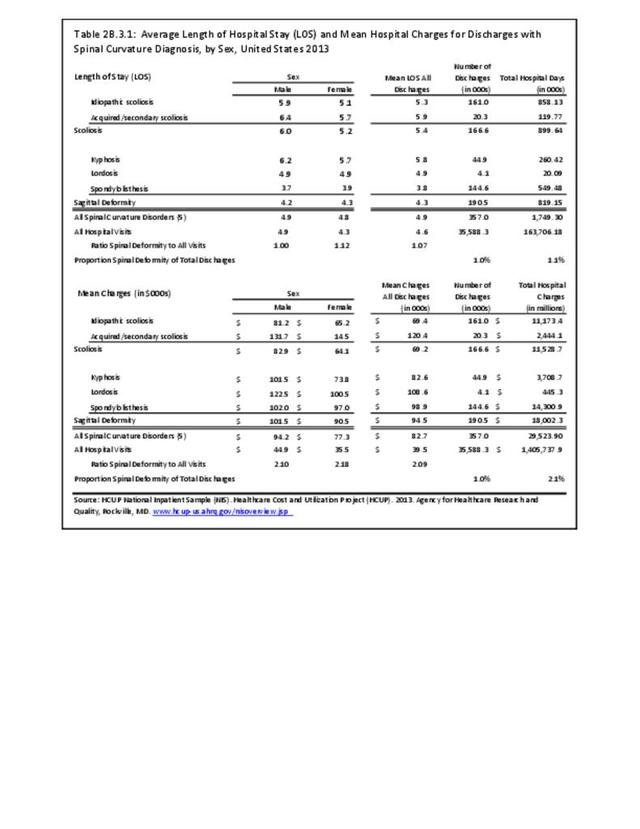
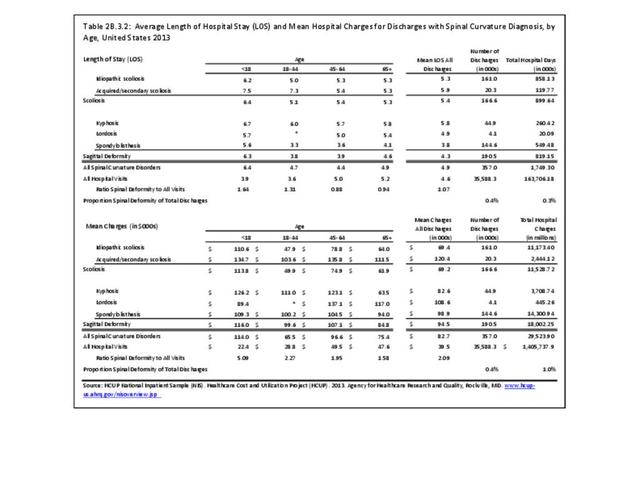
The national mean cost of a hospitalization, including surgical treatment, for patients with a primary diagnosis of sagittal imbalance was $94,500 in 2013 for an average hospital stay of 4.3 days. The HCUP NIS database does not provide hospitalization costs associated with secondary discharge diagnoses, and does not include fees to doctors, tests, and other typical charges associated with hospitalization. Therefore, the most conservative estimate of only hospital charges for adult sagittal imbalance in 2013 was an estimated $18.0 billion (166,600 hospitalizations). Charges are not necessarily actual costs paid. Mean charges for sagittal imbalance diagnosed patients are significantly higher than for all hospital discharge patients. (Reference Table 2B.3.2 PDF CSV)
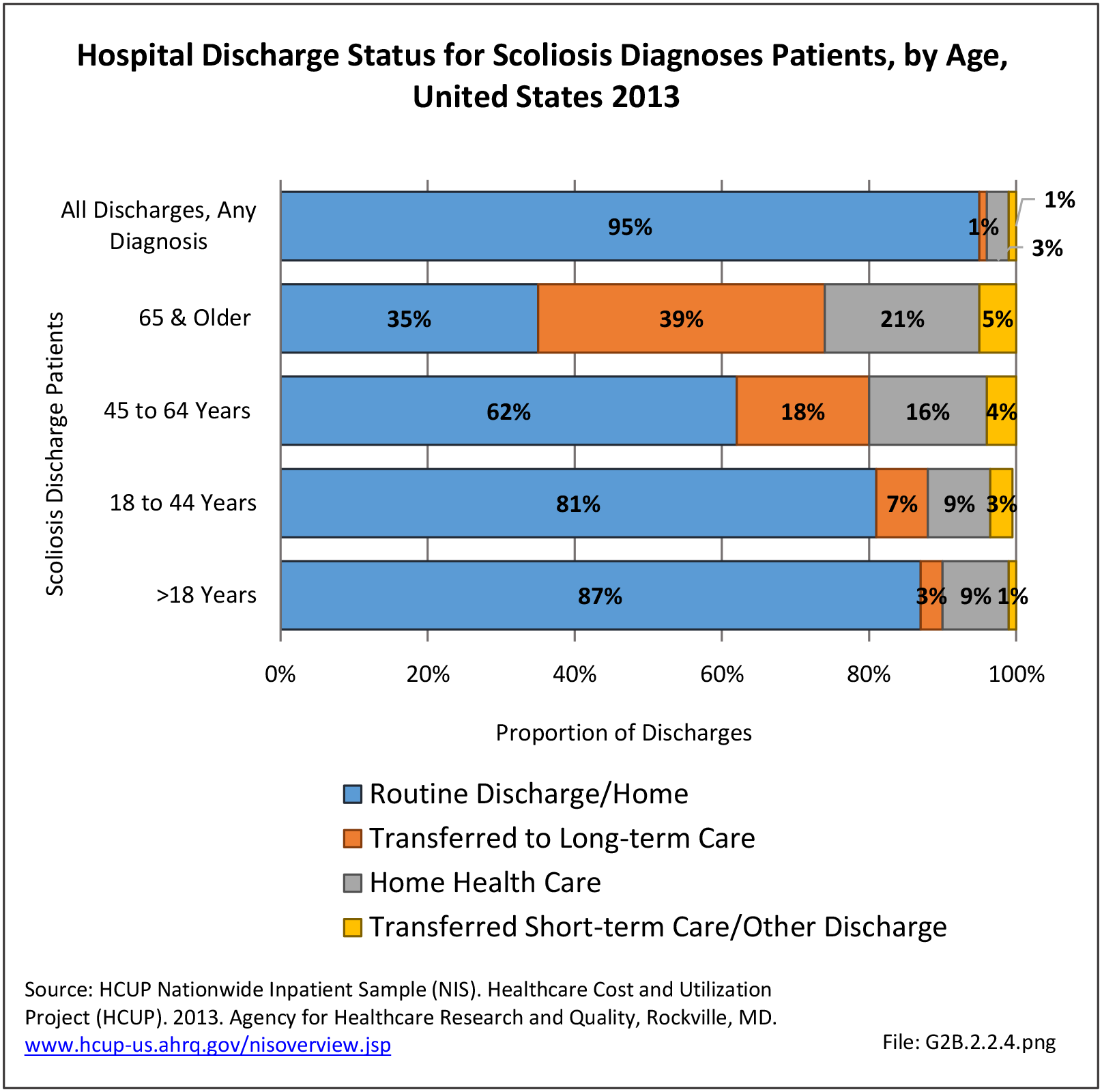
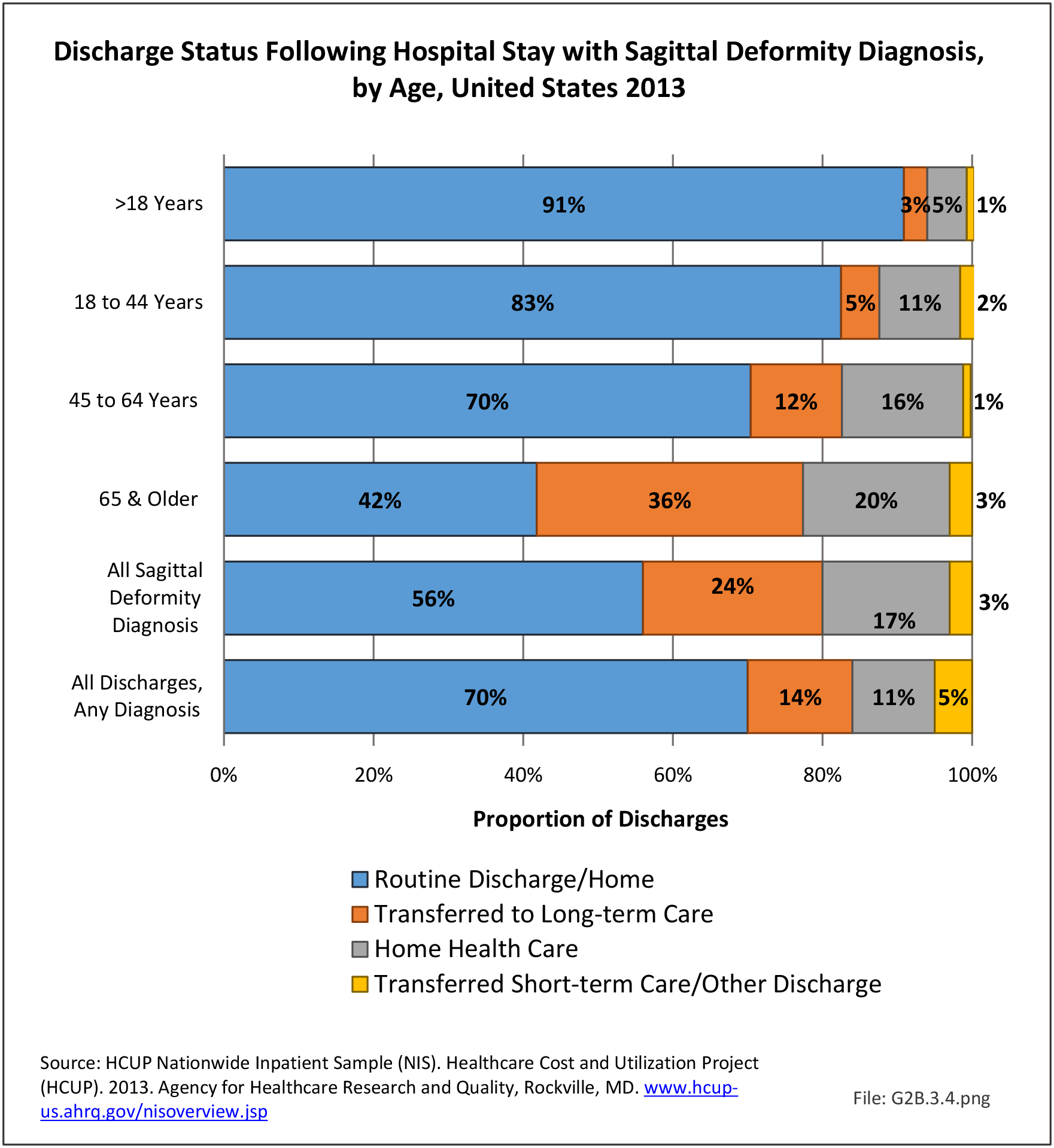
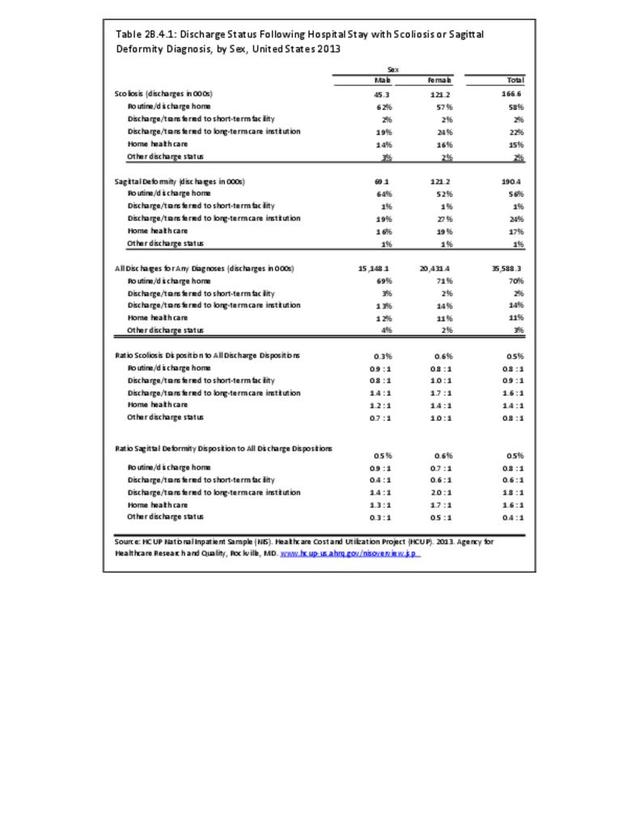
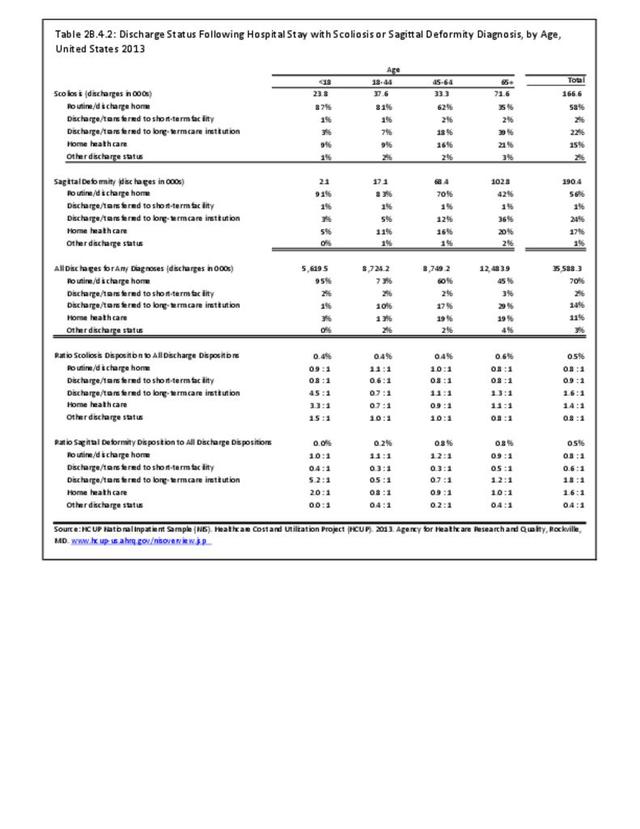
In 2013, slightly more one-half (56%) of patients with a sagittal imbalance diagnosis were discharged to home, compared to 70% of patients with any diagnosis. Patients with a sagittal imbalance diagnosis are more likely to be transferred to a skilled nursing or intermediate care facility (long-term care) than are patients with all other diagnoses. This is particularly true for the elderly population, with 36% of persons age 65 and older with a sagittal imbalance diagnosis moving to a long-term care facility. (Reference Table 2B.4.2 PDF CSV)
The real cost of the management of adult sagittal imbalance to our healthcare system is significant, and the value of care measured by change in health status remains incompletely defined for both nonsurgical and surgical care.
- 1. a. b. c. Makhni MC, Shillingford JN, Laratta JL, et al. Restoration of Sagittal Balance in Spinal Deformity Surgery. J Korean Neurosurg Soc 2018;61(2):167–179. doi:10.3340/jkns.2017.0404.013.
- 2. Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976) 2005;30:1082–1085.
- 3. a. b. c. Roussouly P, Nnadi C. Sagittal plane deformity: an overview of interpretation and management. Eur Spine J 2010:19(11);1824-1836.
- 4. Moshirfar A, Rand FF, Kebaish KM. Fixed sagittal plane deformity: causes, prevention, and treatment options. Seminars in Spine Surgery 2011:23(2);135-141.
- 5. Cavanilles-Walker JM, Ballestero C, Iborra M, Ubierna MT, Tomasi SO. Adult Spinal Deformity: Sagittal Imbalance. International Journal of Orthopaedics 2014:1(3).
- 6. Lamartina C, Berjano. Classification of sagittal imbalance based on spinal alignment ad compensatory mechanisms. European Spine Journal 2014:23(6):1177-1189.
Edition:
- Fourth Edition