A growing body of work on health-related knowledge translation1 reveals significant gaps between what is known to improve health, and what is done to improve health.
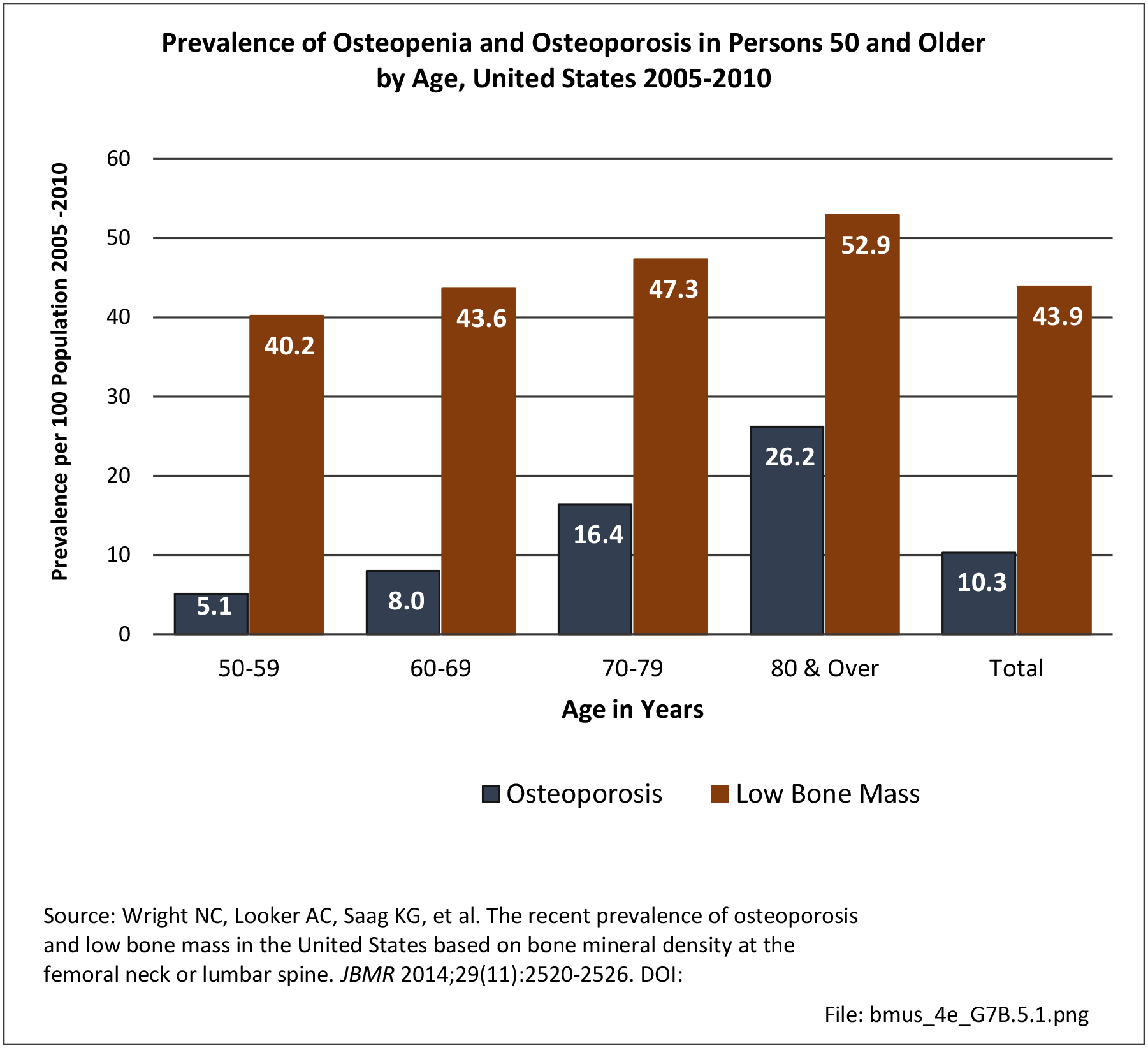
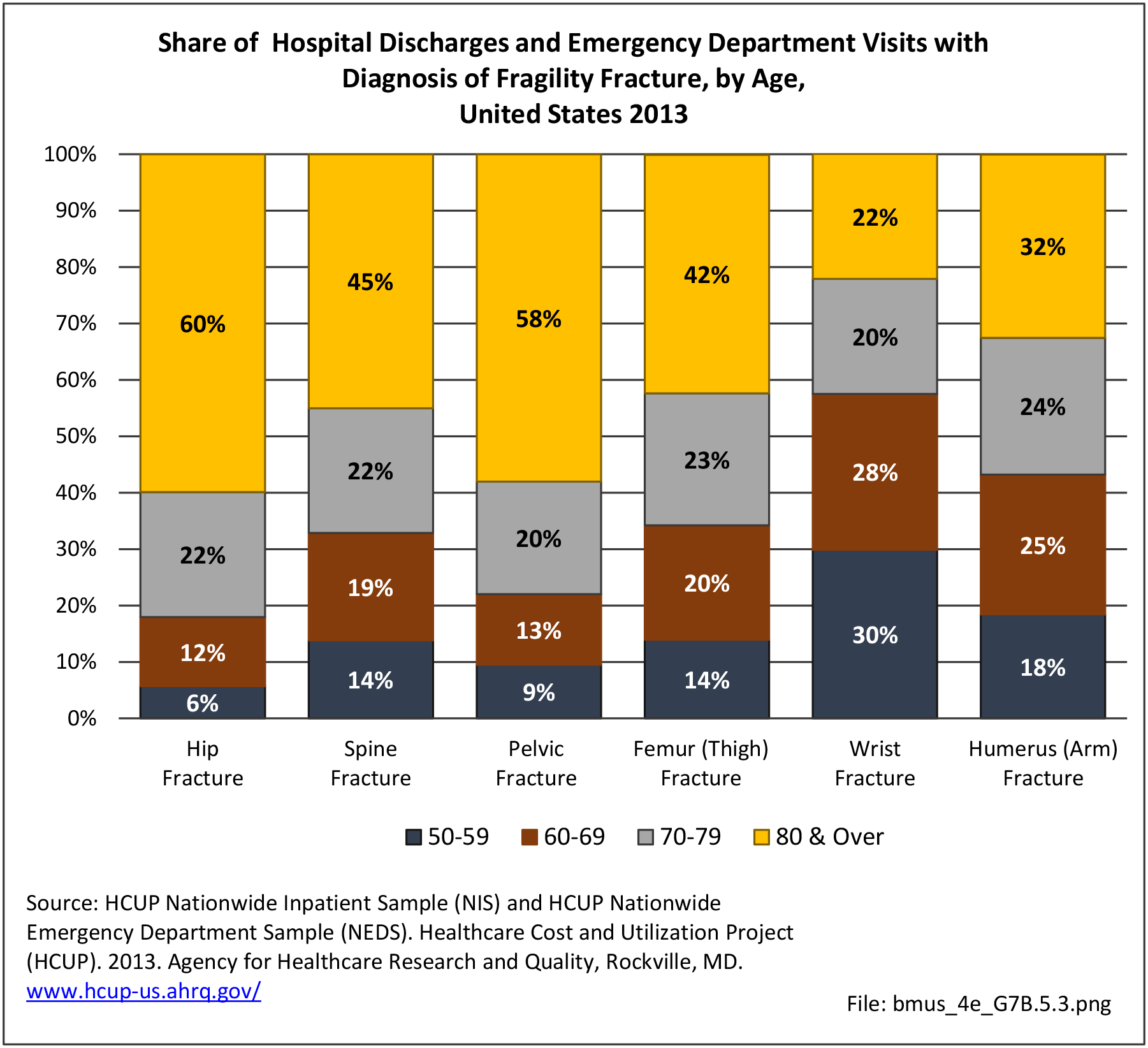
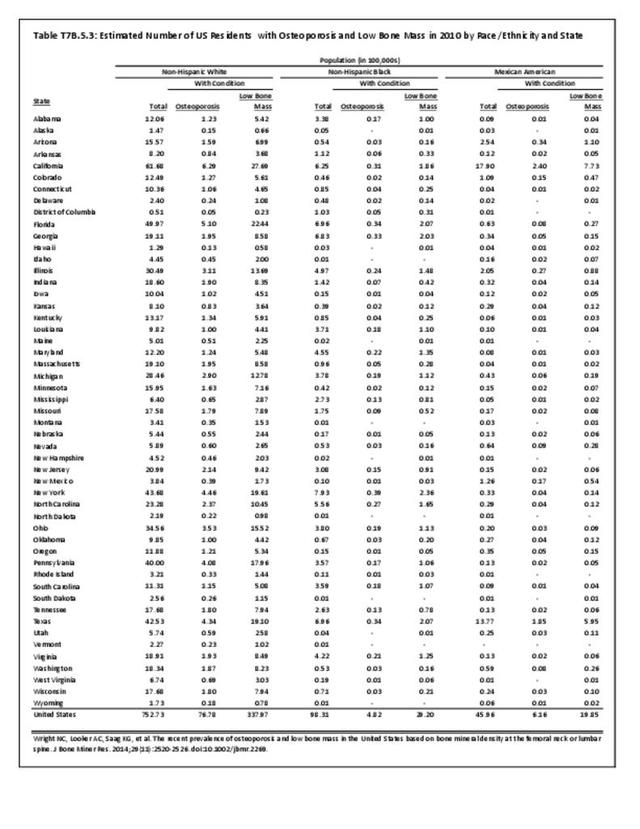
A gap in medical care continues to occur after an osteoporosis related fracture in older adults. Furthermore, the decreasing rate of treatment for osteoporosis after hip fracture is noted in the US by Solomon and colleagues.2 The latest quality measures by the National Commission on Quality Assessment (2017) indicate that treatment for osteoporosis after a fracture in an older woman has increased. Evaluation measured as a bone density test is performed in 72.7% of health management organizations (HMOs) and 82% of Preferred Provider Organizatons (PPO). Actual osteoporosis treatment is reported as 46.7% of HMOs and 39.1% of PPOs. This is a substantial increase over prior annual findings.
System-based quality improvement programs such as the American Orthopaedic Association’s “Own the Bone” have been successful with raising awareness and spearheading improvement in increasing treatment rates for osteoporosis after a fracture.3,4,5
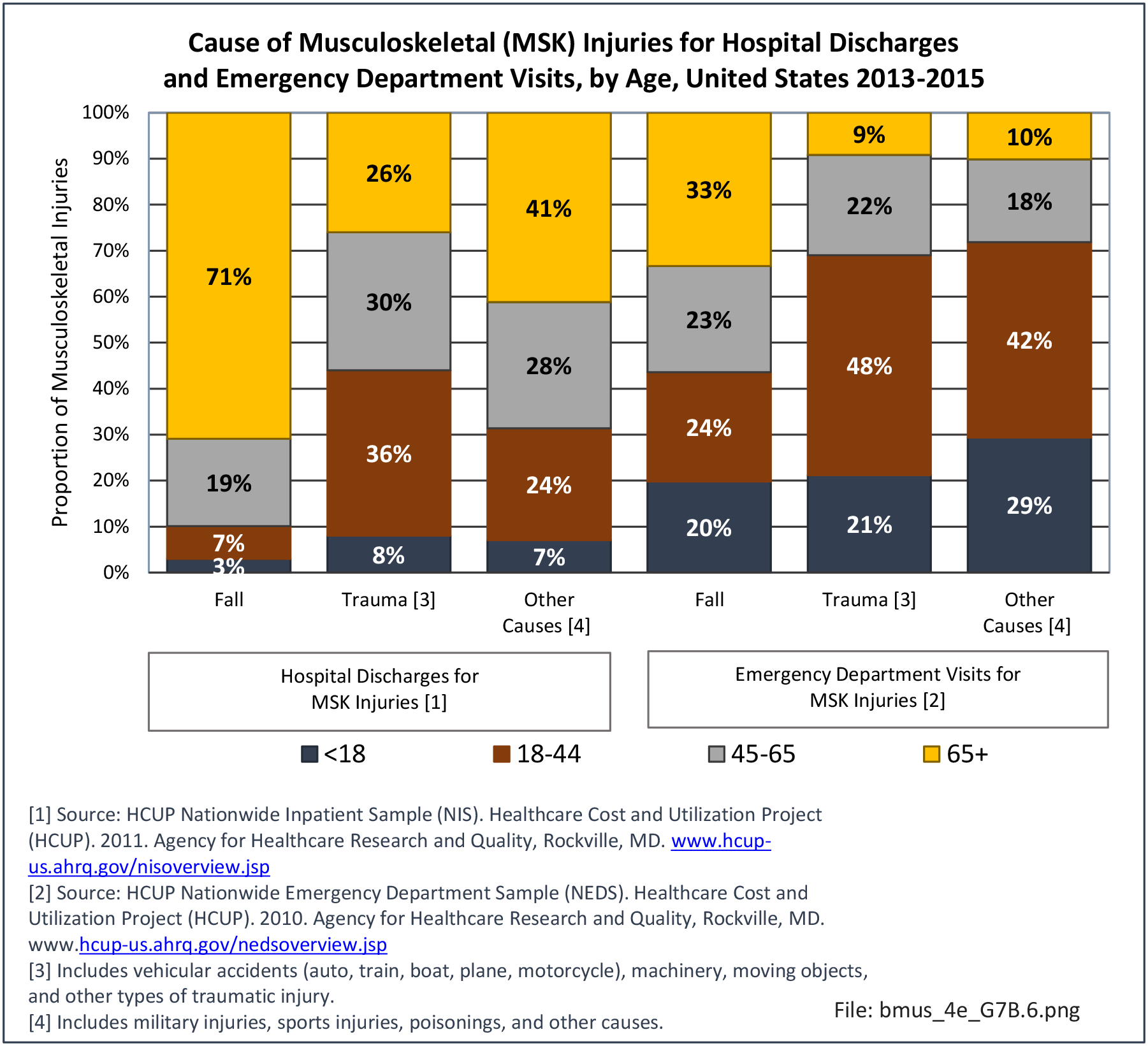
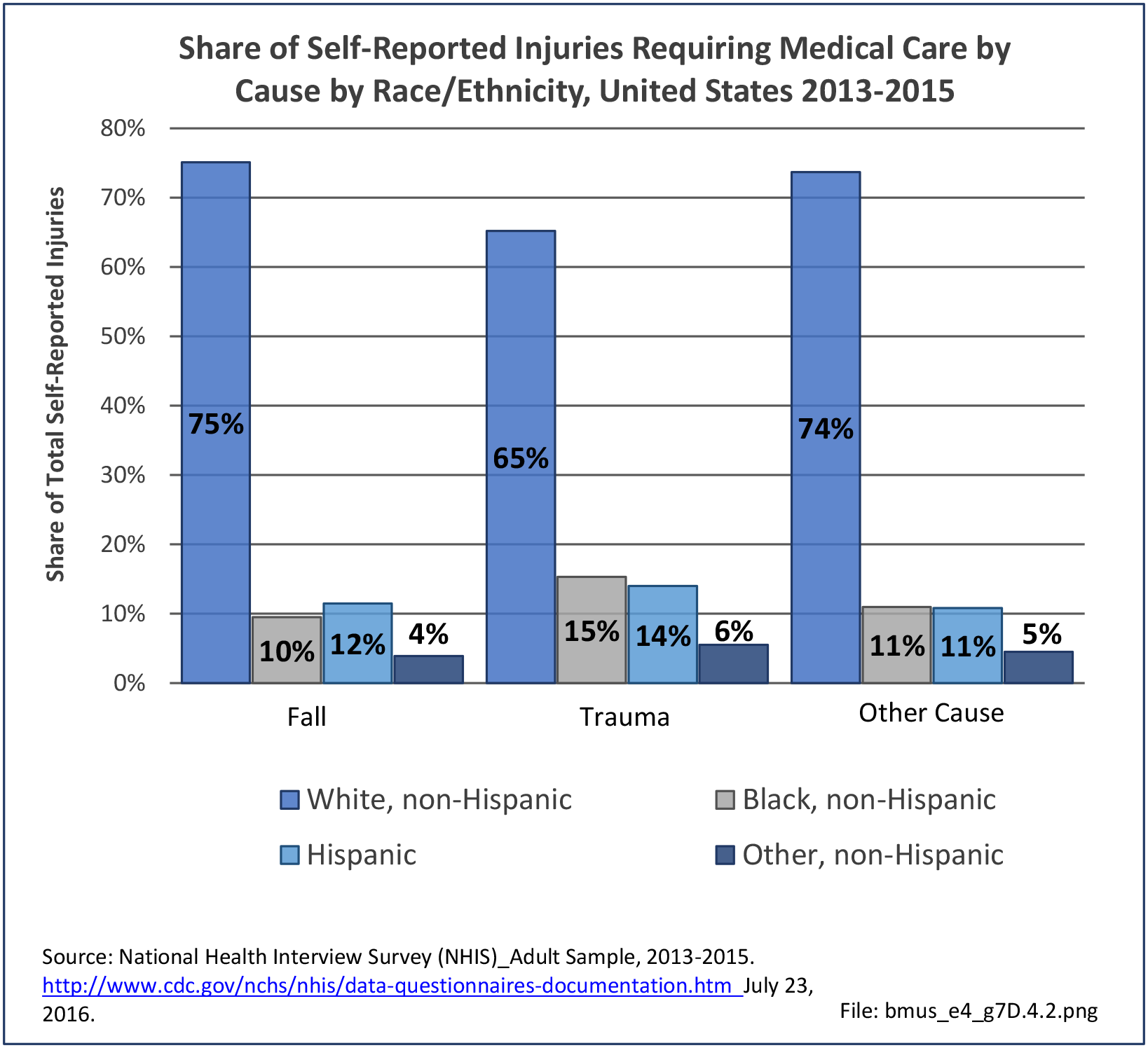
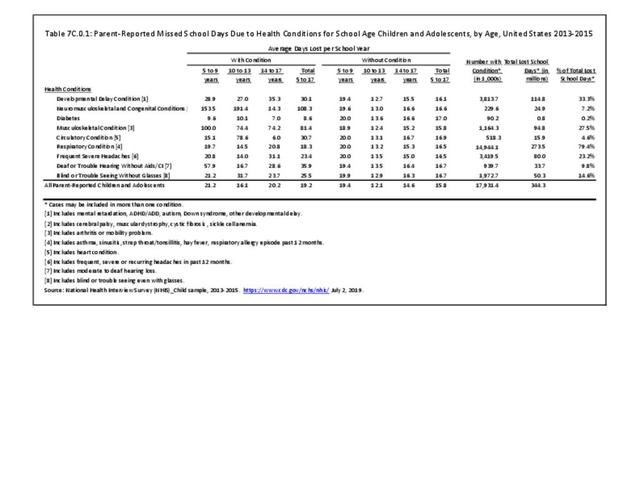
Another area with a gap in medical care is in the prevention in falls. Falls are common in older individuals, affecting as many as 30% of older women. Injuries from falls include fractures and blunt head trauma, and result in increased mortality. Women with self-reported osteoarthritis (OA), in particular, have an increased risk of falls, and in spite of elevated bone mass, remain at risk of fractures.6 In 2017, the cost of fall injuries totaled as much as $49.5 billion, depending on methods used to identify a fall, the national healthcare database used, and study design.7 As the population ages, the financial toll for older adult falls is projected to reach $67.7 billion by 2020.8
Falls result in more than 2.8 million injuries treated in emergency departments annually, including over 800,000 hospitalizations and more than 21,000 deaths. Every 11 seconds, an older adult is treated in the emergency room for a fall. Every 19 minutes, an older adult dies after a fall.8
In conclusion, musculoskeletal disorders are prevalent, and often of serious consequences in older adults. A greater awareness in osteoporosis care after a fracture can be helped through bone density testing. The use of osteoporosis therapy afater fracture will result in a higher quality of life and prevention of disability among America’s seniors.
- 1. Activities involved in moving research from the laboratory, the research journal, and the academic conference into the hands of people and organizations who can put it to practical use
- 2. Solomon DH, Johnston SS, Boytsov NN, et al. Osteoporosis medication use after hip fracture in U.S. patients between 2002 and 2011. JBMR 2014;29(9):1929-1937.
- 3. Edwards BJ, Bunta AD, WB M, et al. Own the bone, a system-based intervention to improve osteoporosis care after fragility fractures. JBMR 2016;98(24):e109.
- 4. Edwards BJ, Koval K, Bunta AD, et al. Addressing secondary prevention of osteoporosis in fracture care: follow-up to "own the bone". J Bone Joint Surg Am 2011;93(15):e87.
- 5. Dell R, Greene D, Schelkun SR, Williams K. Osteoporosis disease management: the role of the orthopaedic surgeon. J Bone Joint Surg Am 2008;90 Suppl 4:188-194.
- 6. Arden NK, Nevitt MC, Lane NE, et al. Osteoarthritis and risk of falls, rates of bone loss, and osteoporotic fractures. Study of Osteoporotic Fractures Research Group. Arthritis Rheum 1999;42(7):1378-1385.
- 7. Haddad YK, Bergen G, Florence C. Estimating the economic burded related to older adult fall by state. J Public Health Manag Pract 2019;25(2);e17-e24.
- 8. a. b. National Council on Aging. Falls Prevention Facts. https://www.ncoa.org/news/resources-for-reporters/get-the-facts/falls-pr... Accessed December 1, 2019.
Edition:
- Fourth Edition