One of the greatest unmet needs related to back pain is the ability to clearly diagnose the source of back pain. There are so many physical and non-physical sources of back pain that patients are often treated inappropriately before they are clearly diagnosed. Thousands of dollars are often spent on diagnostic evaluations without finding a clear source of back pain, a process that needs to be broken by earlier diagnosis, earlier definitive treatment, and maintenance of the ability to continue working.
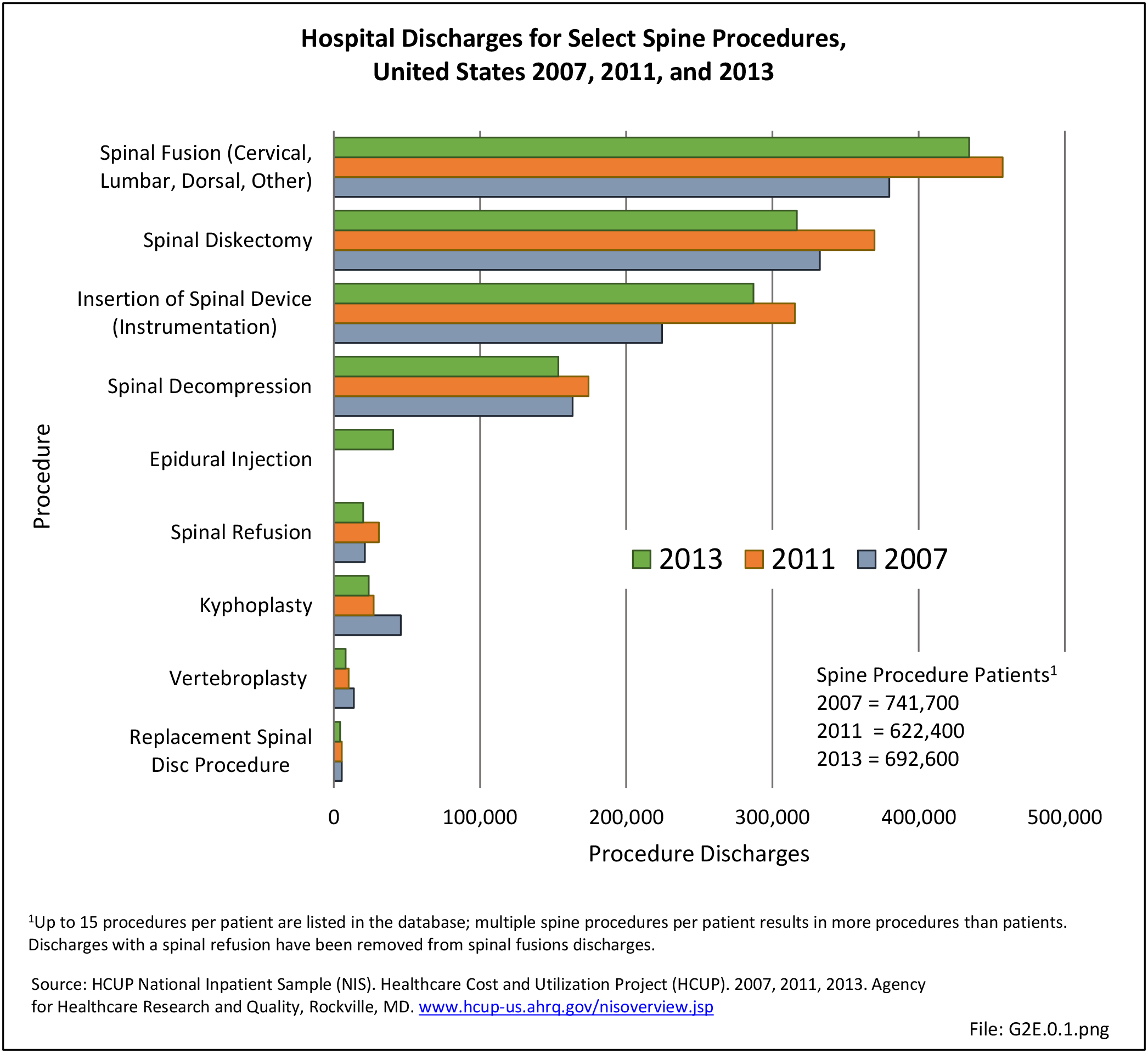
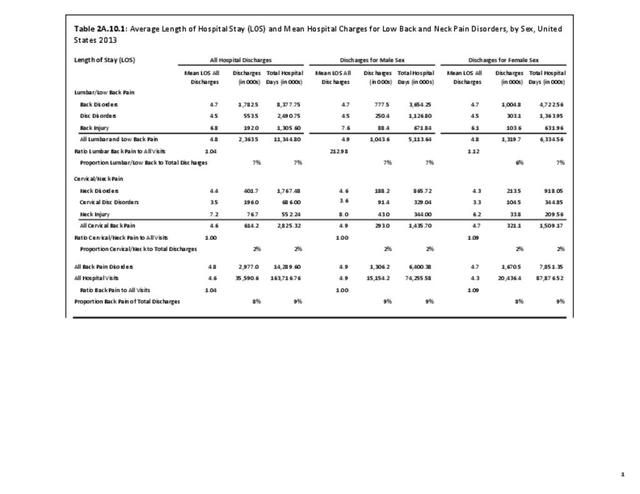
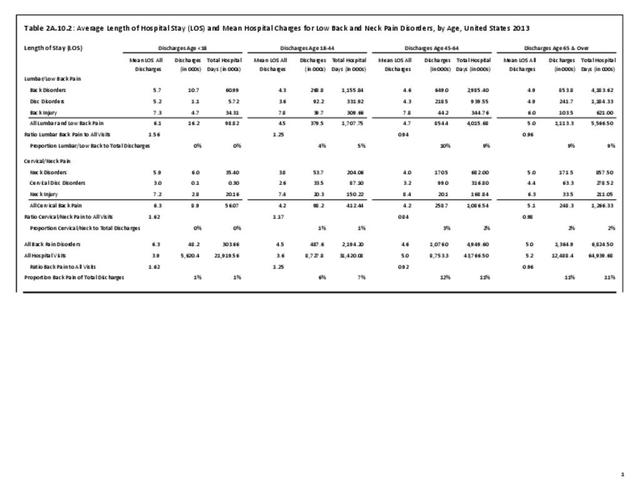
Most patients with back and neck pain are treated non-operatively, often with alternative treatments, including such treatments as acupuncture, homeopathy, and massage. We know that enormous amounts of money are spent on many of these treatments, yet no quantifiable measures of cost or effect are yet available. Furthermore, the lack of information about treatments by chiropractors, physical therapists, and other care providers results in underestimated cost estimates for treatment of low back pain. There is also a lack of information on medical procedures done in offices or surgicenters, limiting estimates of cost and effectiveness of many interventional procedures, including many surgical procedures. These gaps in knowledge should be filled to obtain accurate estimates of the impact of back and neck pain on society.
As such, there remains debate regarding the most effective treatment for low back pain. Increased recommended alternatives to non-surgical options adds credence for improved informed consent, creating conversation about benefits and risks and leading to a better shared decision making process for the patient. Though research is limited, per Zaina et al, informing the patient of anticipated outcomes of not only surgery but other options is vital. In a systematic review performed by Zaina et al, the authors evaluated the effectiveness of different types of surgery compared with different types of non-surgical intervention in the treatment of low back pain secondary to lumbar spinal stenosis (LSS).1 The authors’ analysis demonstrated no differences in pain-related disability improvement between surgical (decompression with or without fusion) and non-surgical care. However, due to the low quality of available studies, the authors were unable to confidently recommend a preferable treatment method for symptomatic LSS.
To begin addressing these needs, there has been an increase in research on the efficacy of non-surgical interventions for low back pain. Ammendolia et al investigated the safety and effectiveness of epidural injections to other treatments for symptomatic LSS.2 Due to the low overall evidence (only 4 randomized controlled trials), the authors were only able to conclude that epidural injections provide improved pain, function, and quality of life for only up to 2 weeks.
Another area of increased interest is the effect of pre- and postoperative spinopelvic parameters (the relationship of the pelvic position to the spine) on treatment outcomes. Several previous investigations have described the magnitude of parameter correction afforded by surgical and non-surgical treatment modalities. However, many of these studies have featured small sample sizes and have rarely offered level I or II evidence. As such, there exists a need for large, prospective studies that investigate the true impact of influence of spinopelvic parameters on treatment outcomes for low back pain.
Acupuncture has been utilized in the treatment of low back pain for centuries, and has recently been established as a non-operative complimentary treatment in the United States.3 A meta-analysis evaluating the use of acupuncture in the treatment of low back pain demonstrated the use of acupuncture as a complimentary, highly cost-effective treatment.4 According to the World Health Organization (WHO) cost-effectiveness threshold values, the cost of complimentary acupuncture treatment was determined to be $48,562 per disability-adjusted life year (DALY) avoided. Interestingly, in patients where comorbid depression was also alleviated at the same rate as pain, the cost was revealed to be $18,960 per DALY avoided. The authors concluded that acupuncture, as a substitute for standard care, was most cost-effective when used in patients with comorbid depression.
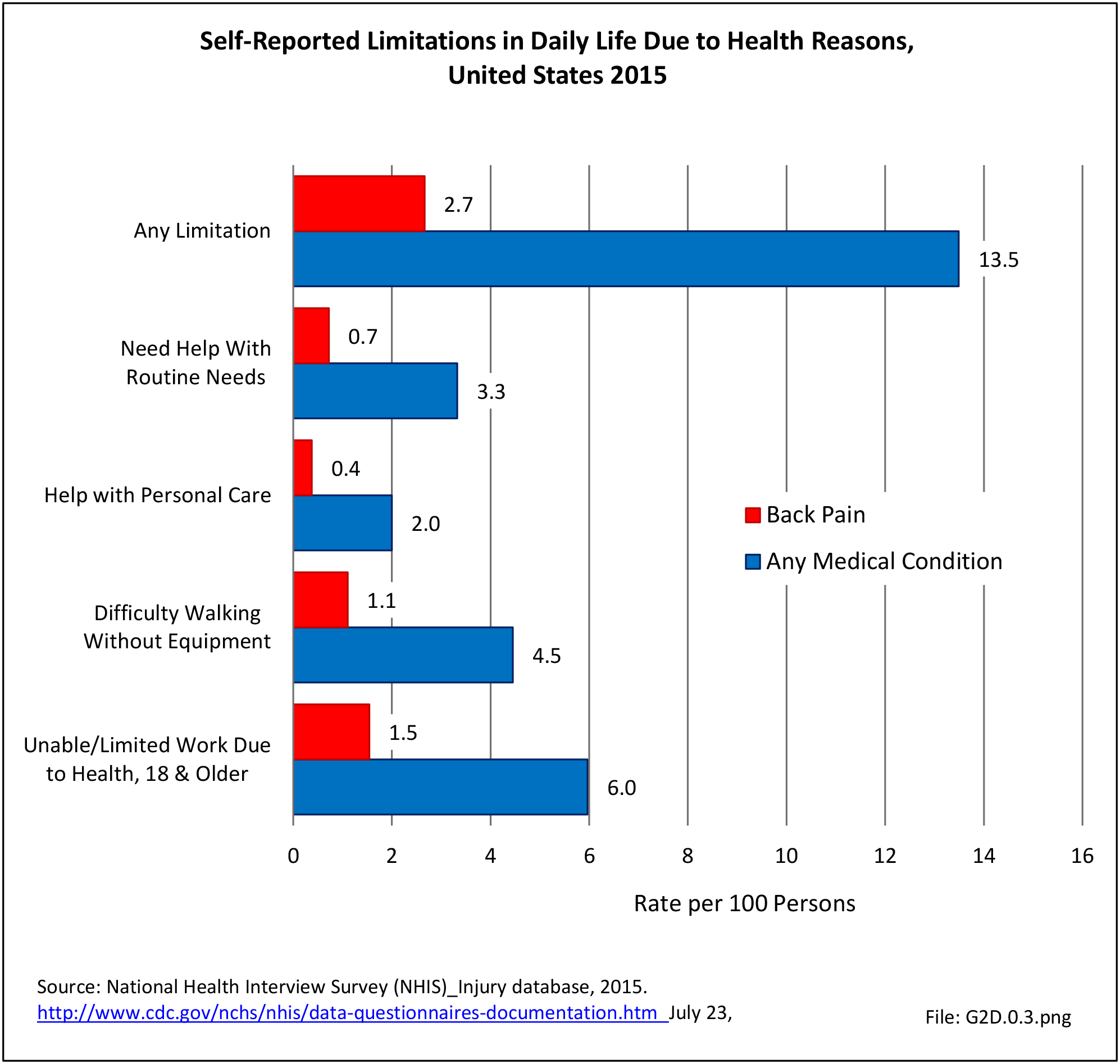
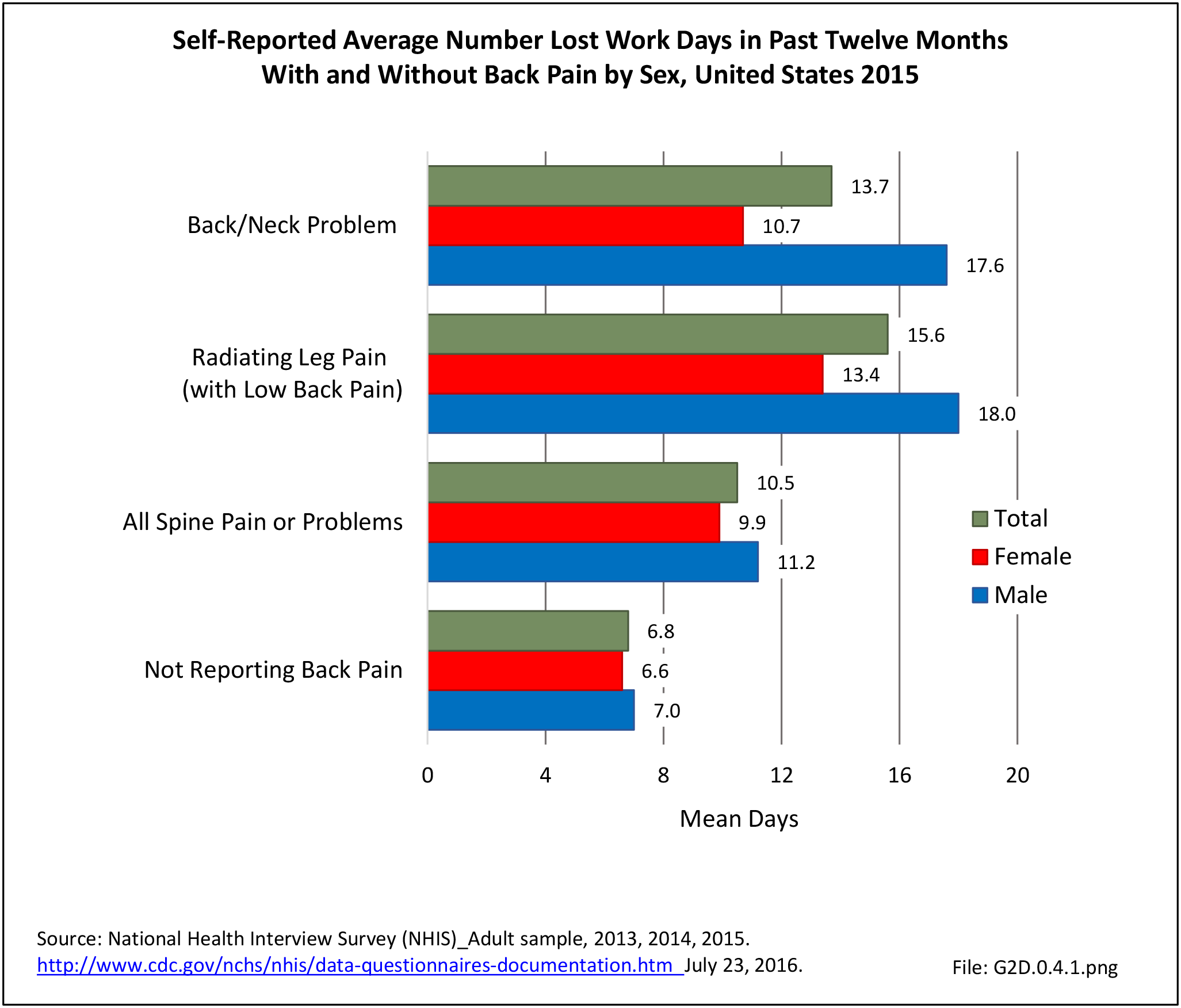
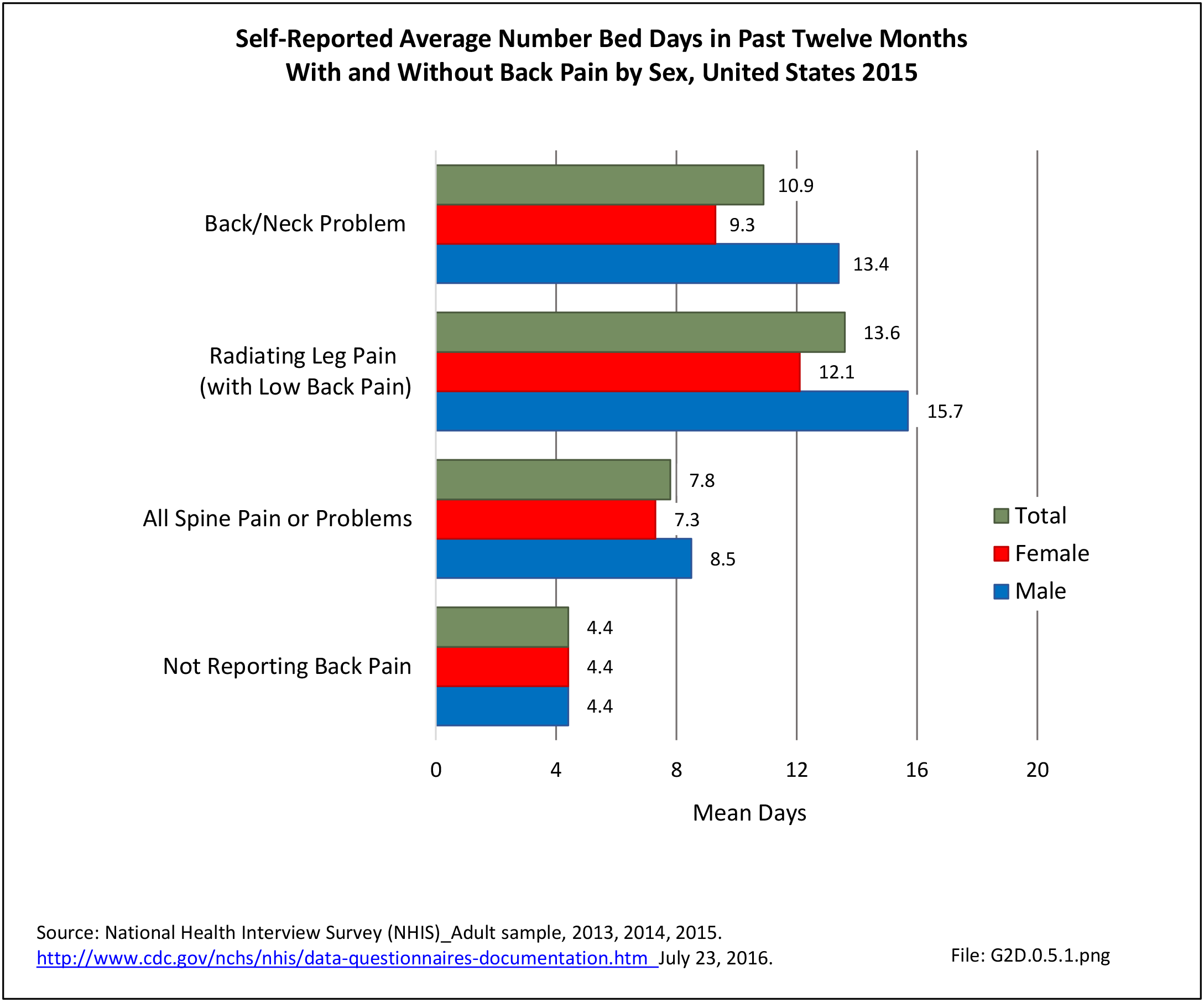
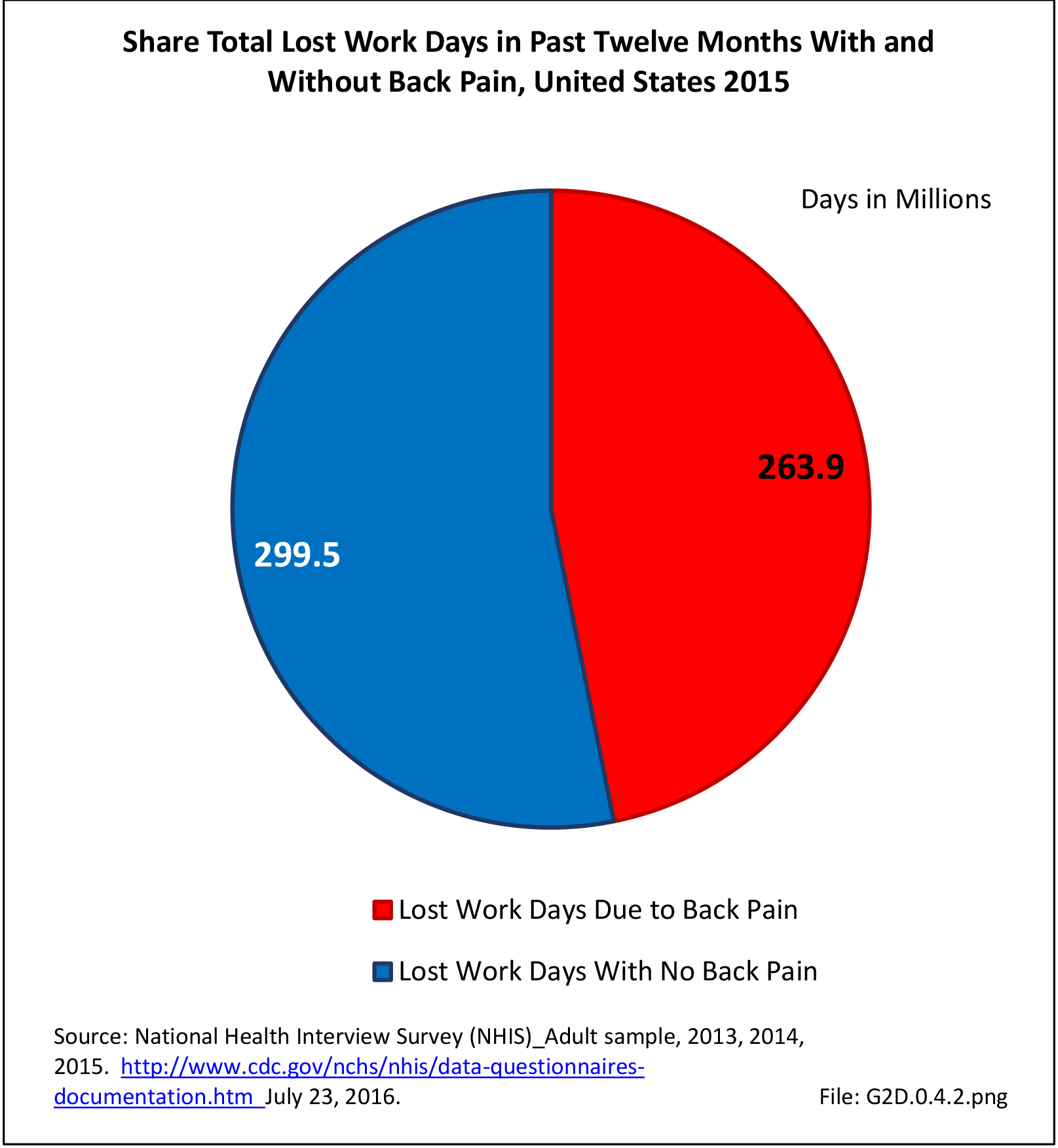
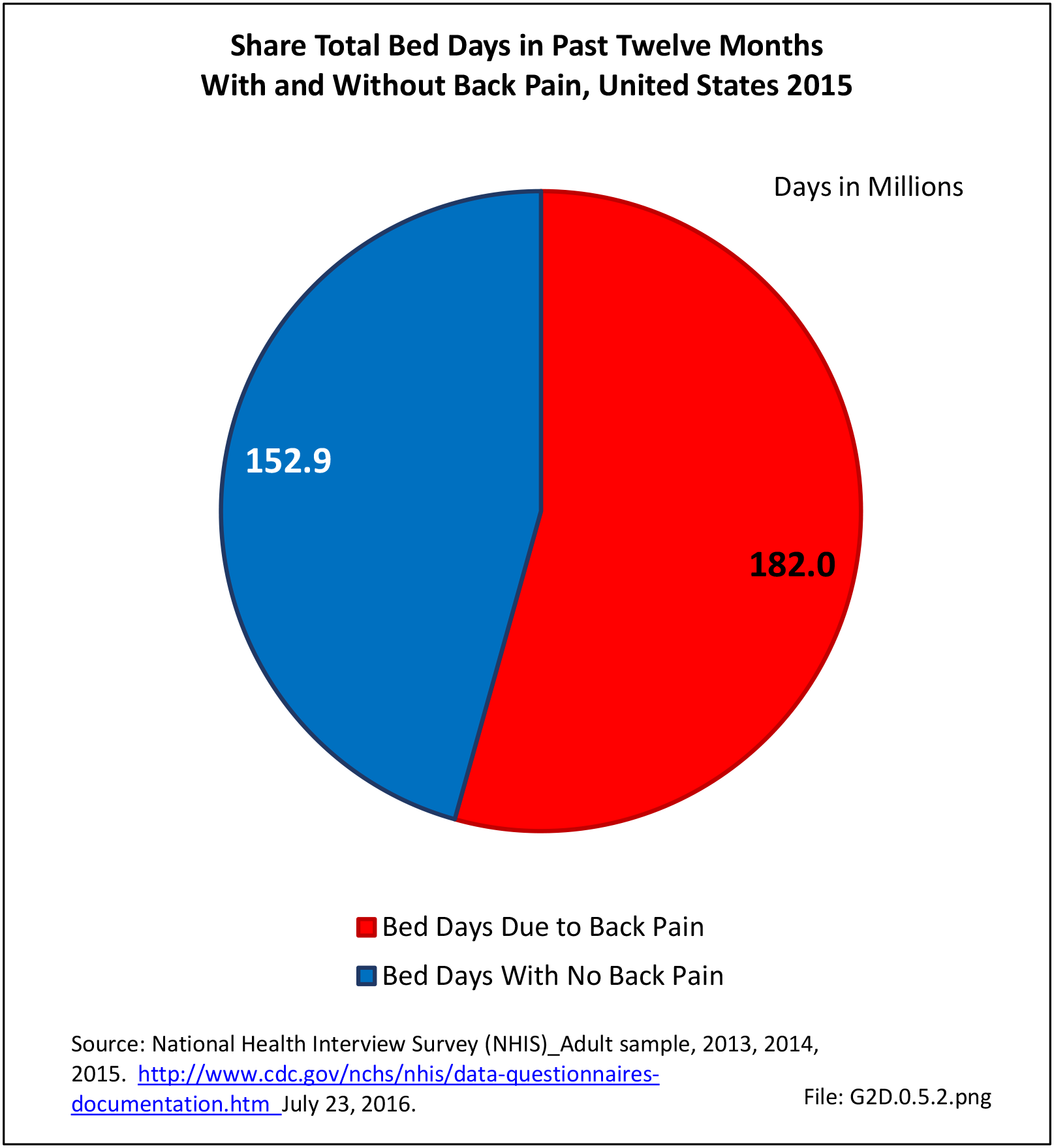
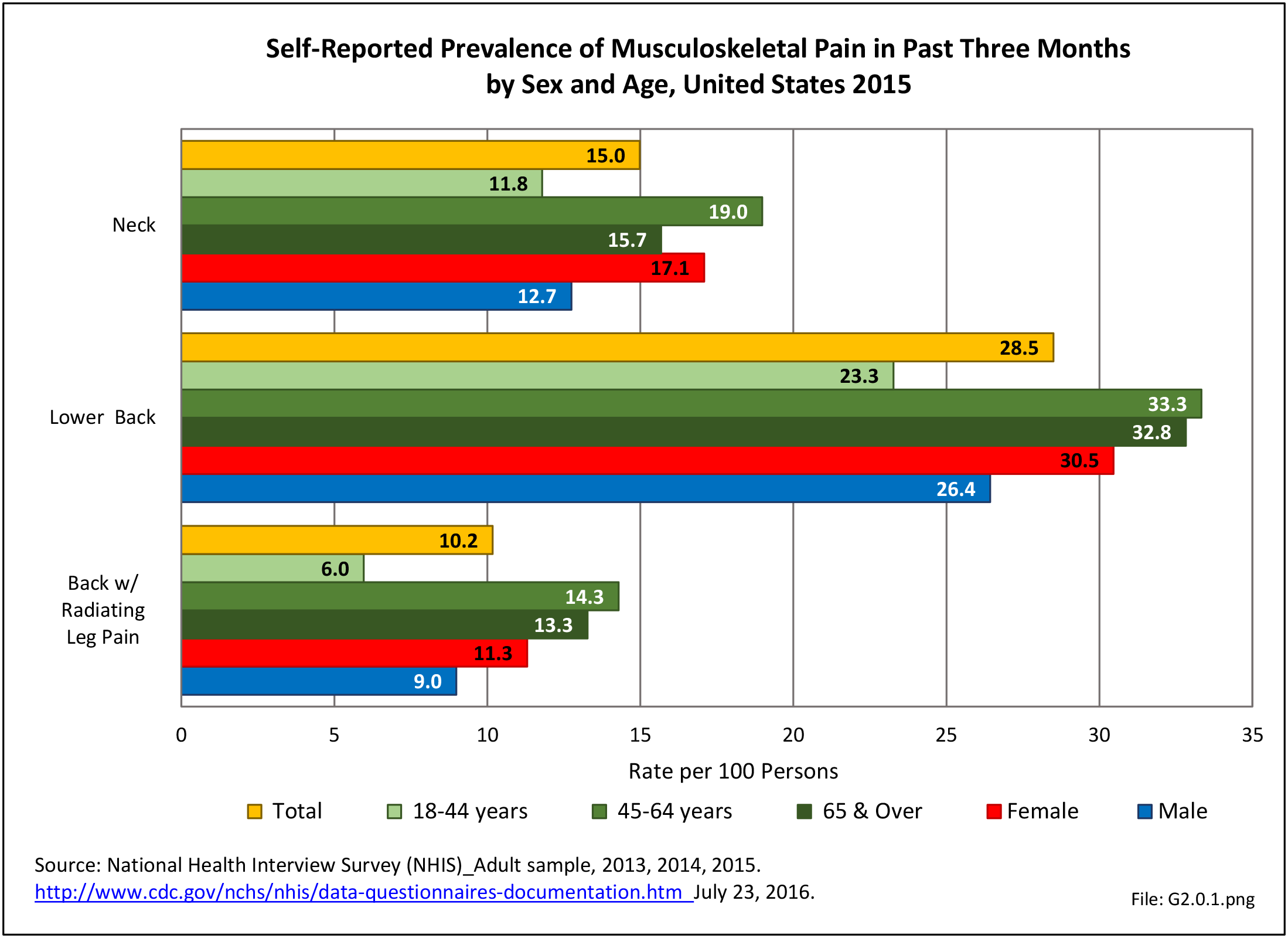
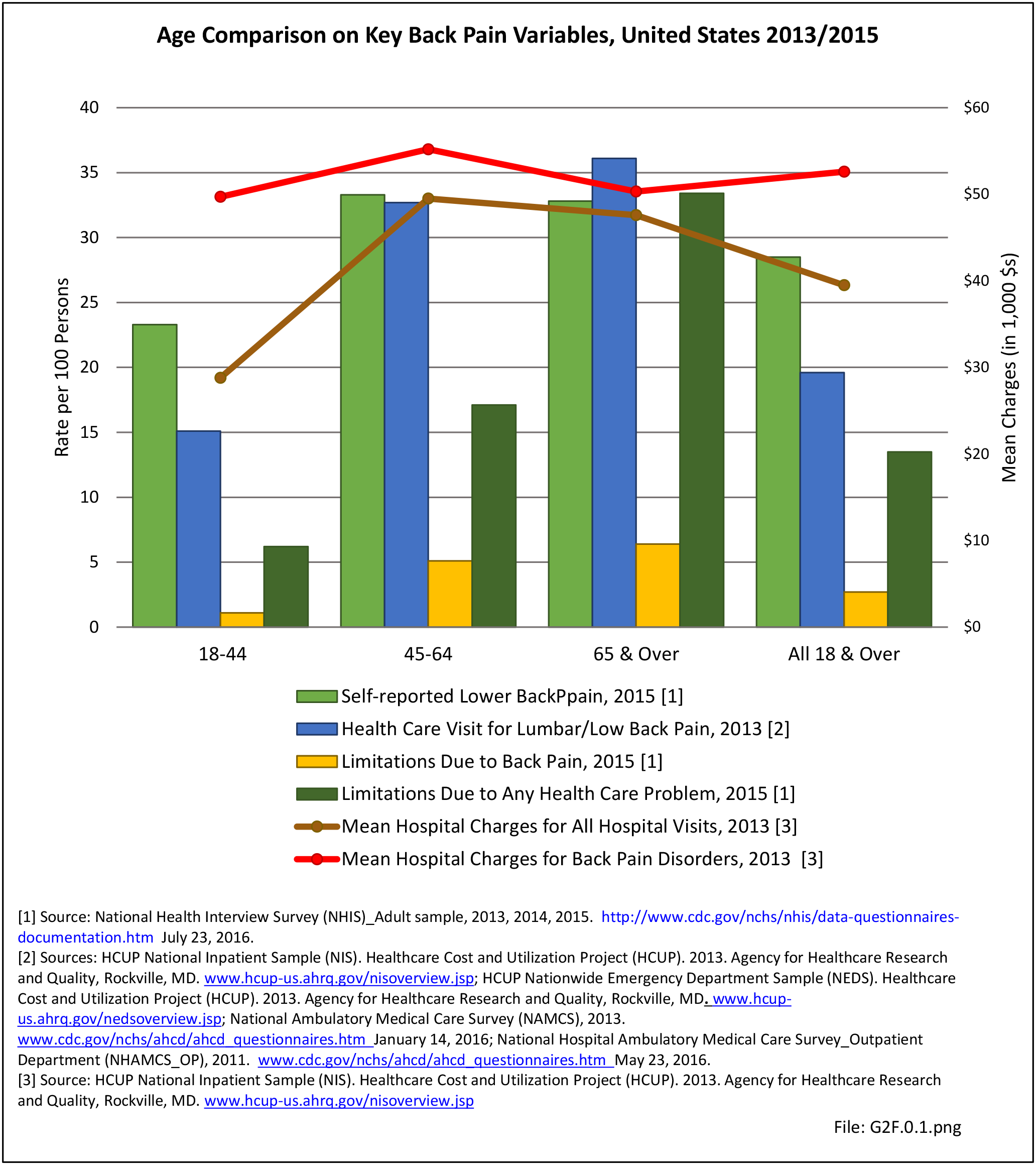
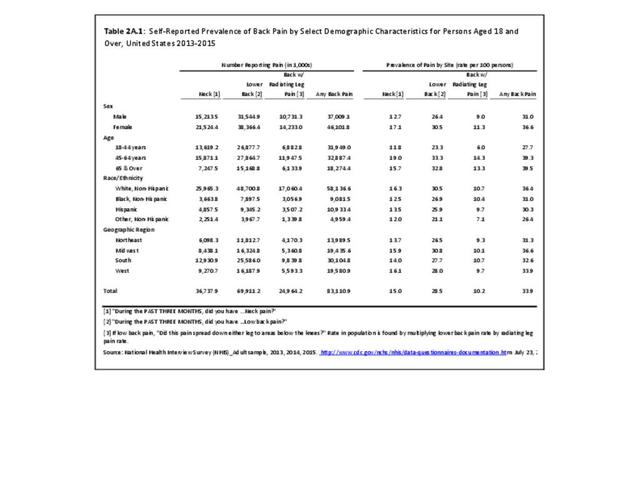
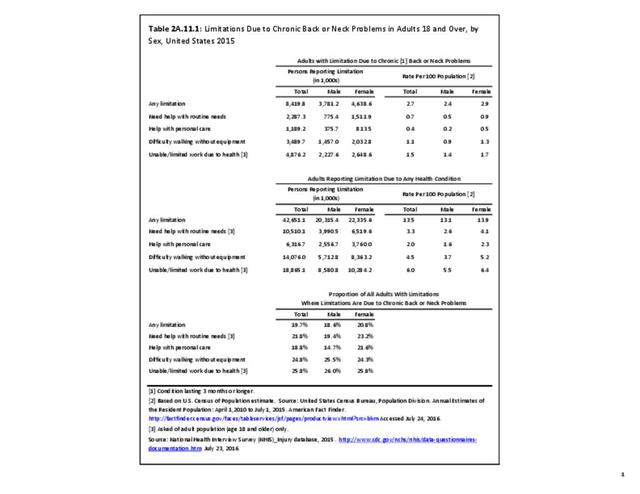
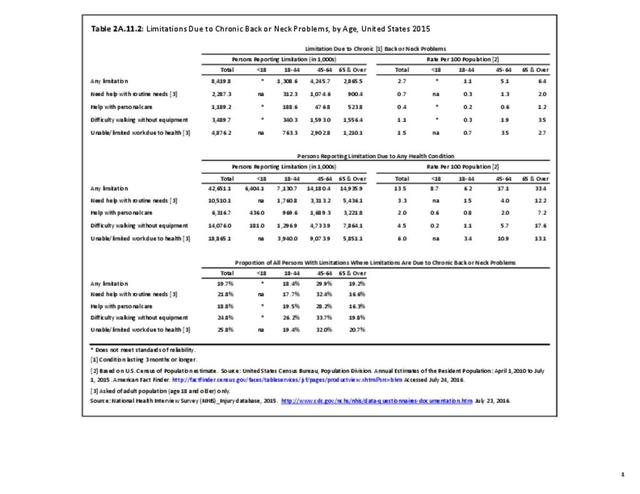
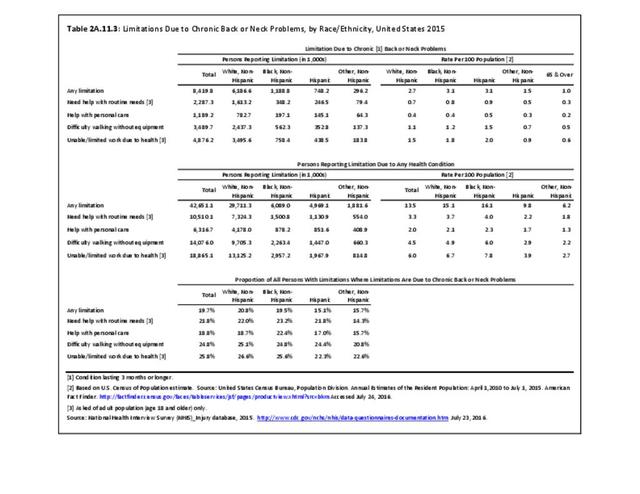
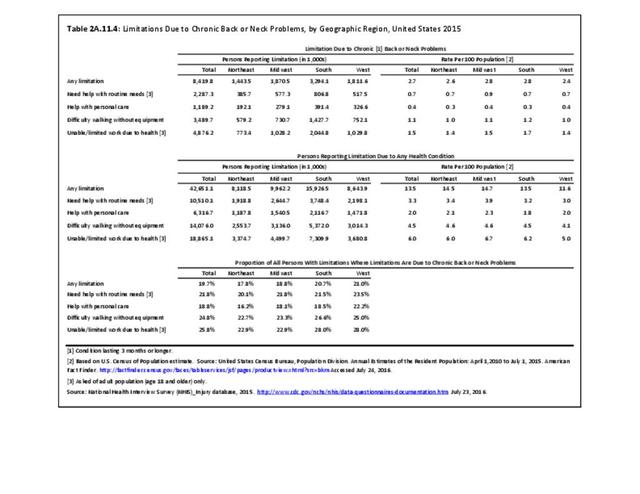
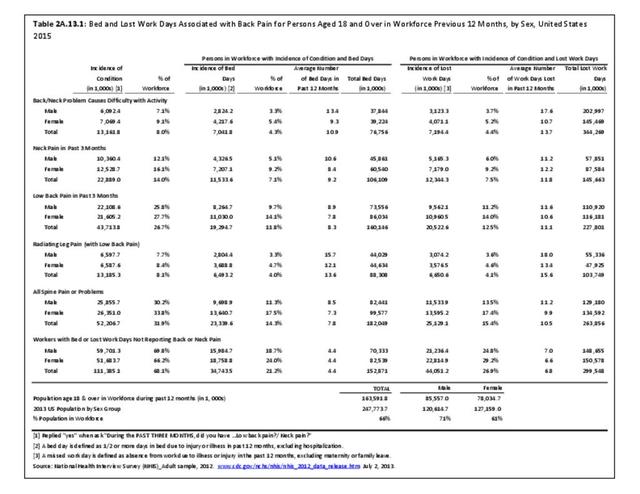
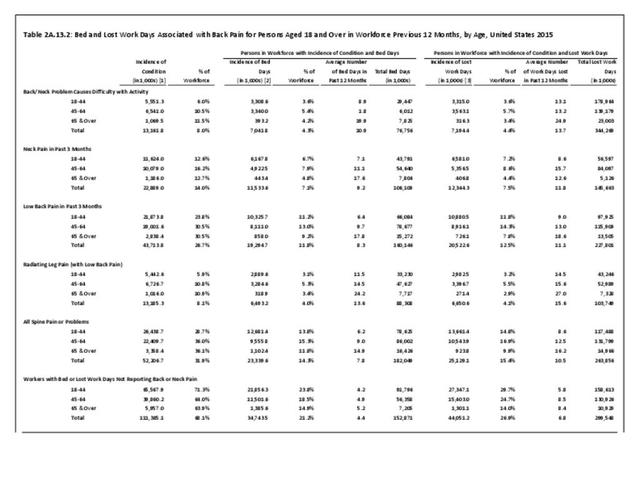
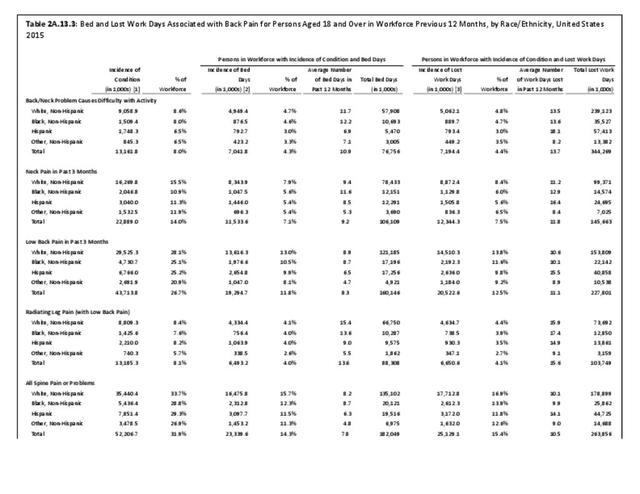
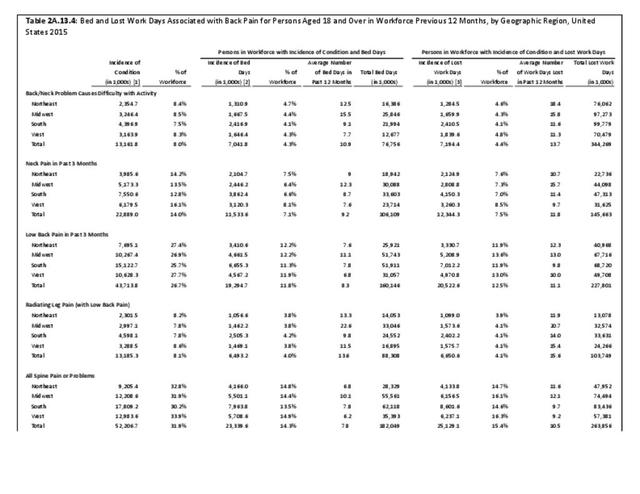
As noted in the previous discussion of Indirect Costs, back pain was the cause of close to 264 million lost work days in a 12-month period during 2014-2015. In addition, over 4%, or 1 in 25, persons in the prime working ages of 18 to 64 report they are either limited in the type or amount of work they can do or are unable to work at all due to back pain. It is clear that back pain has a substantial impact on the workforce, and that finding ways to reduce or repair causes of back pain is needed. (Reference Table 2A.11.2 PDF CSV)
In general, there is a need for high quality clinical research in treatment of low back pain. This includes addressing the lack of evidence for best practices for non-surgical active care approaches and surgical treatment. Additionally, work-related back pain has the potential to become "chronic" back pain, often with co-morbid dependence on narcotic pain medications. This process needs to be broken by earlier diagnosis, maintenance of ability to continue working, and earlier definitive treatment.
There is a need to promote a culture of "stopping back pain before it starts" by adopting spine care procedures, such as proper posture and balance exercise regimes, by persons of all ages as a counter to back pain. In addition to BMUS, the World Spine Care and Global Spine Care Initiative are coalitions all working to find ways to reduce back pain and back pain costs.
- 1. Zaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016(1):CD010264.
- 2. Ammendolia C, Stuber KJ, Rok E, et al. Nonoperative treatment for lumbar spinal stenosis with neurogenic claudication. Cochrane Database Syst Rev. 2013(8):CD010712.
- 3. Chao R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American College of Physicians and the American Pain Society Ann Intern Med. 2007;147(7):478-491.
- 4. Taylor P, Pezzullo L, Grant SJ, Bensoussan A. Cost-effectiveness of acupuncture for chronic nonspecific low back pain. Pain Pract. 2014;14(7):599-606.
Edition:
- Fourth Edition