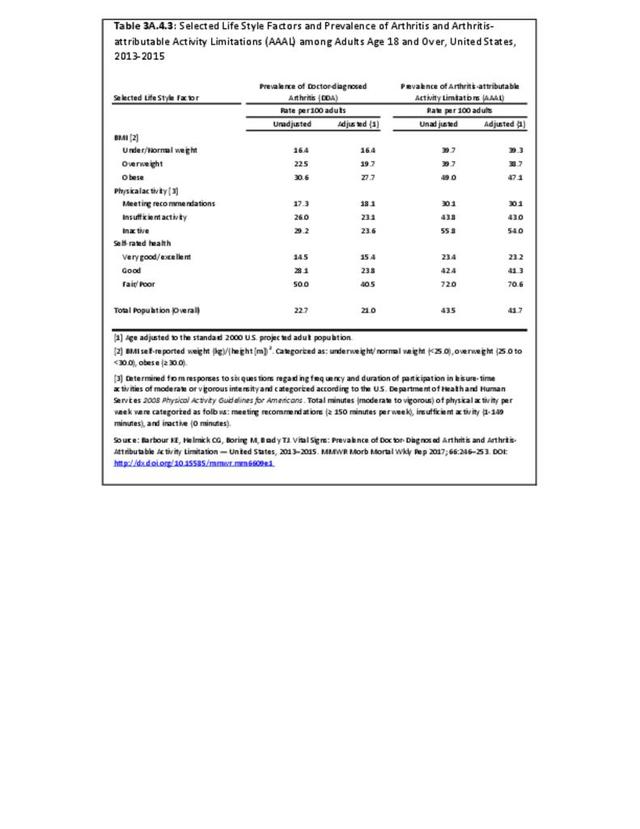
There are widespread and consistent professional recommendations for most types of AORC that involve increasing self-management of the disease through education, physical activity, and achieving a healthy weight, but little progress is being made.1 Such behavioral interventions offer evidence-based improvements to patients without the side effects seen with medications and other interventions. While most clinical settings are not set up to help patients achieve these recommendations effectively, increasing clinical/community linkages may offer a better approach. To see if provider referrals to community resources is a better solution, approaches such as the 1.2.3 Approach to Provider Outreach and Spread the Word: Marketing Self-Management Education Through Ambassador Outreach are being pilot tested in communities.
The Healthy People project started with the 1979 Surgeon General’s report, Healthy People: The Surgeon General’s Report on Health Promotion and Disease Prevention. The current version of Healthy People 2020 has set nine arthritis objectives for the nation to achieve by 2020, but only limited progress has occurred with the current level of investments in interventions. Currently, four new developmental objectives are included in the Arthritis, Osteoporosis, and Chronic Back Conditions topic area as part of a larger effort to insure that chronic pain, regardless of the original cause, is included in Healthy People 2020.
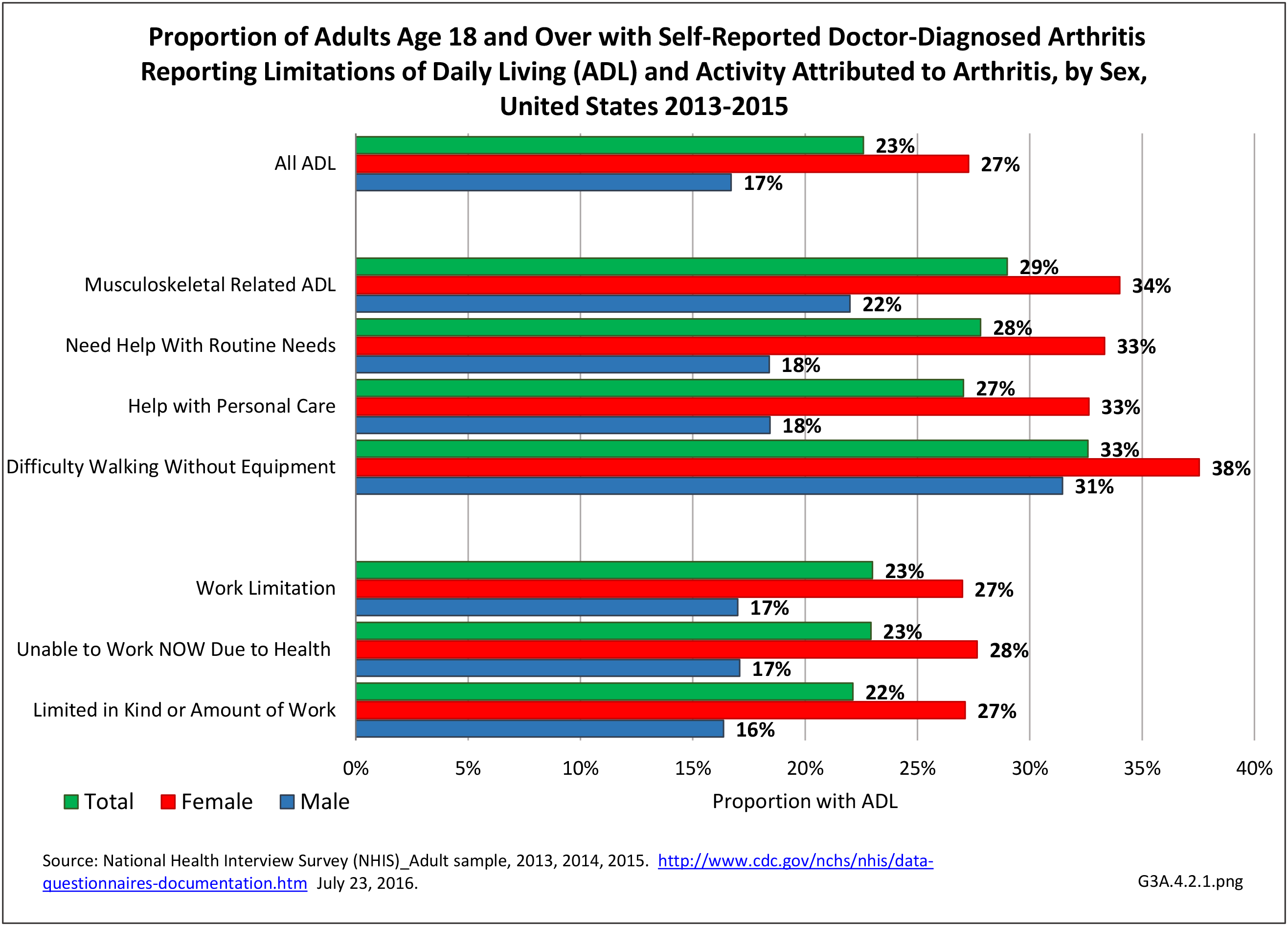
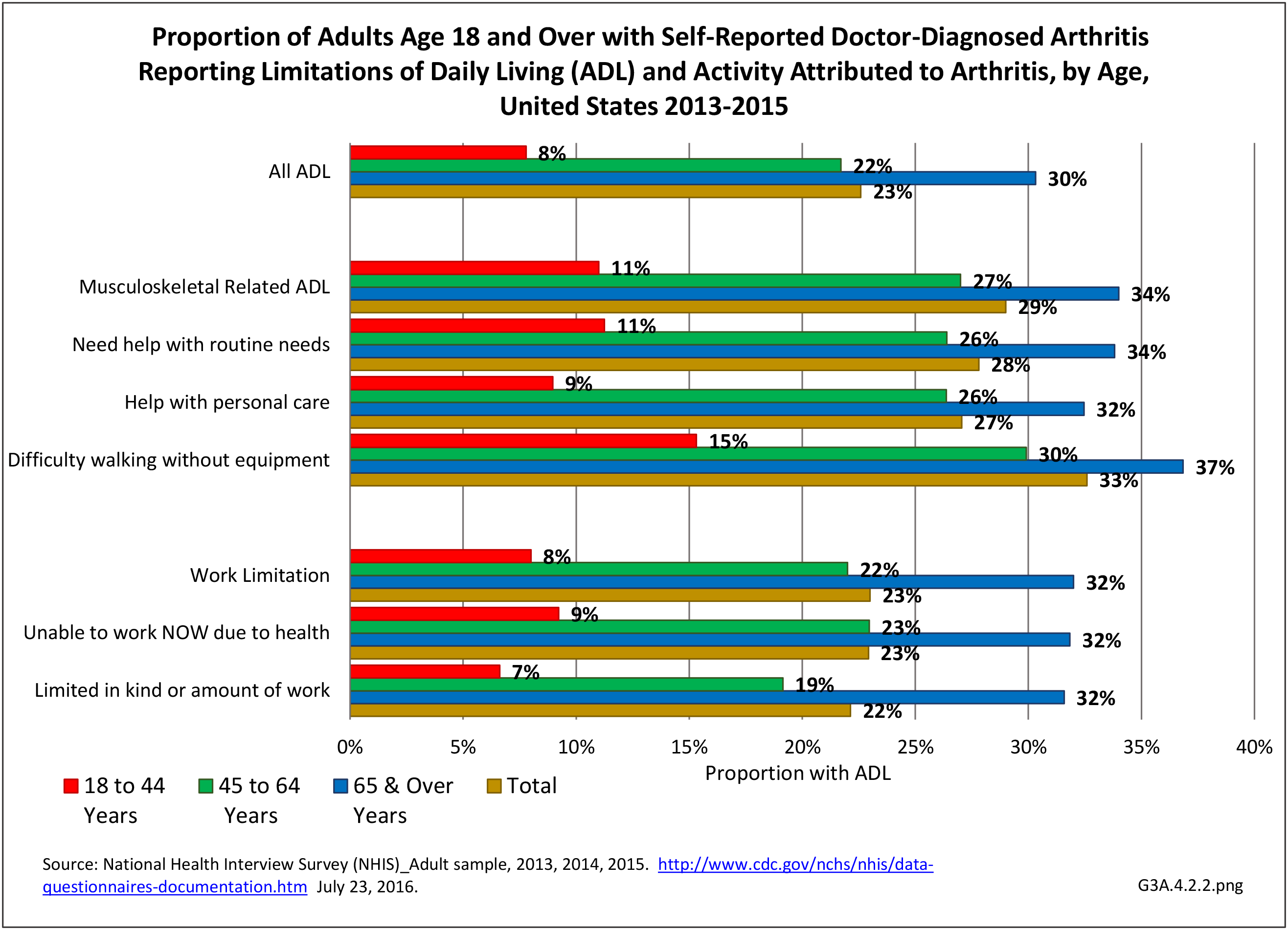
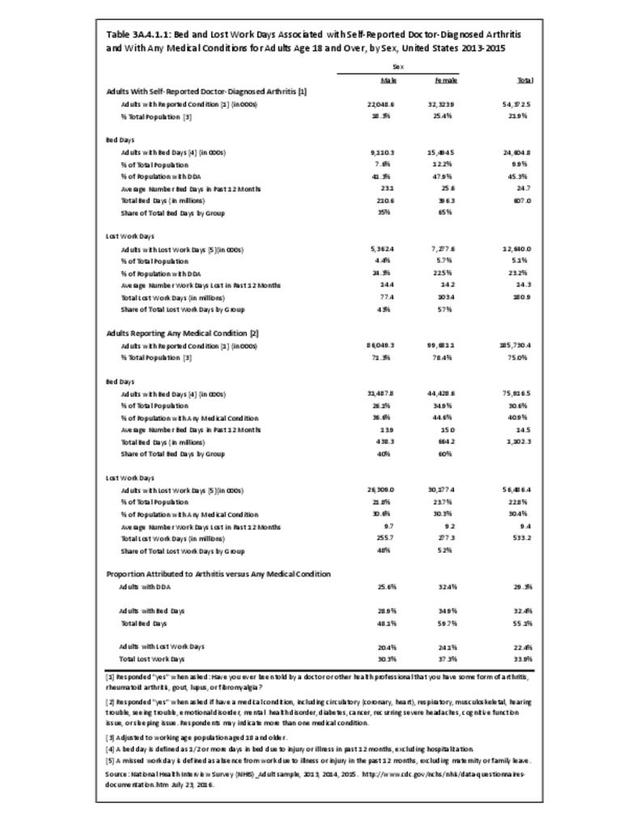
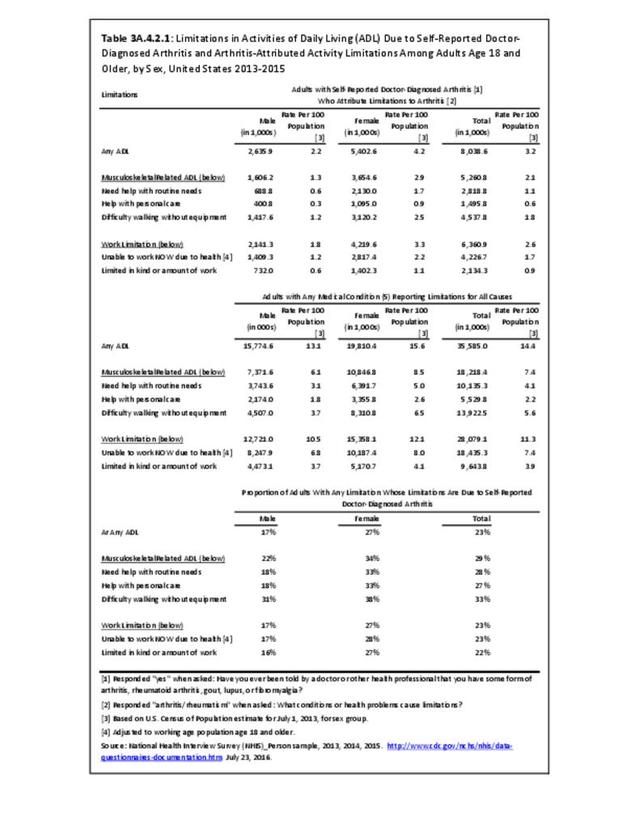
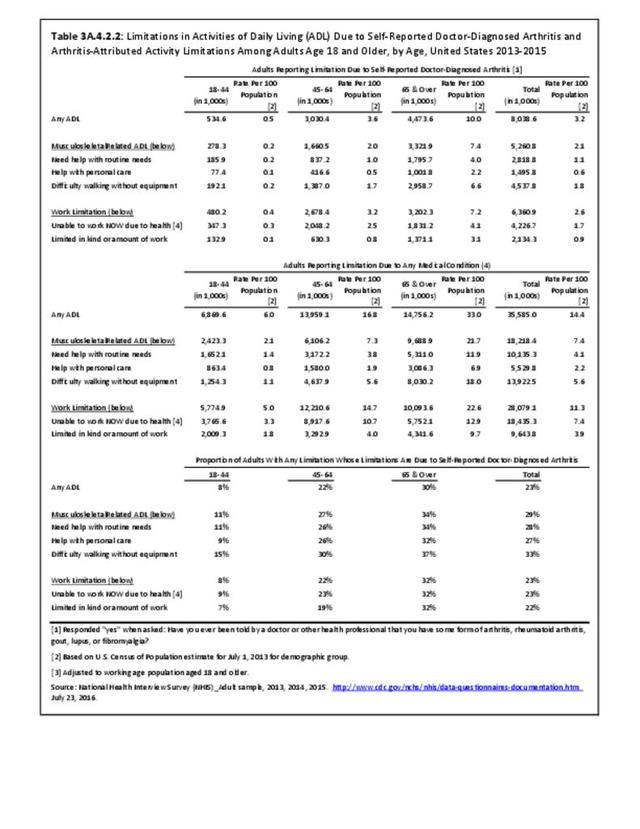
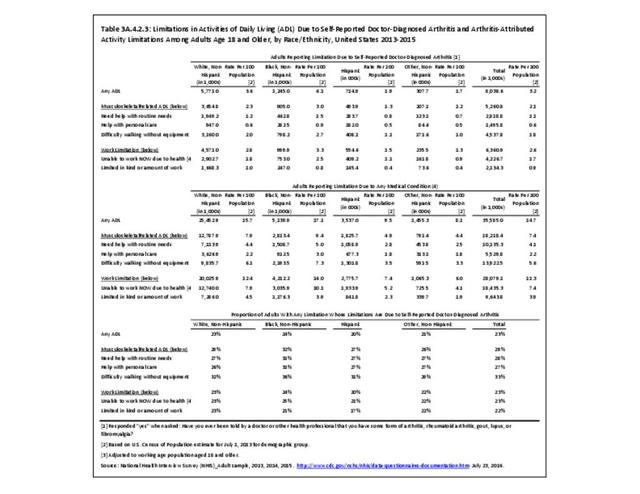
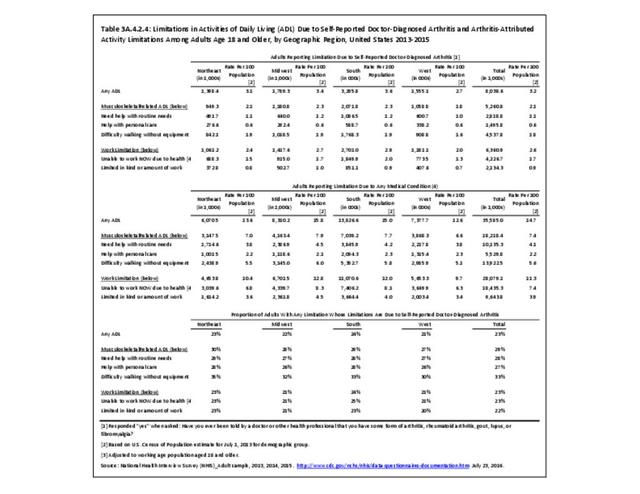
There is a need for more conveniently measured outcomes that are important to most people. Such outcomes include effects on work, activities, health-related quality of life, independence, and ability to keep doing valued life activities.
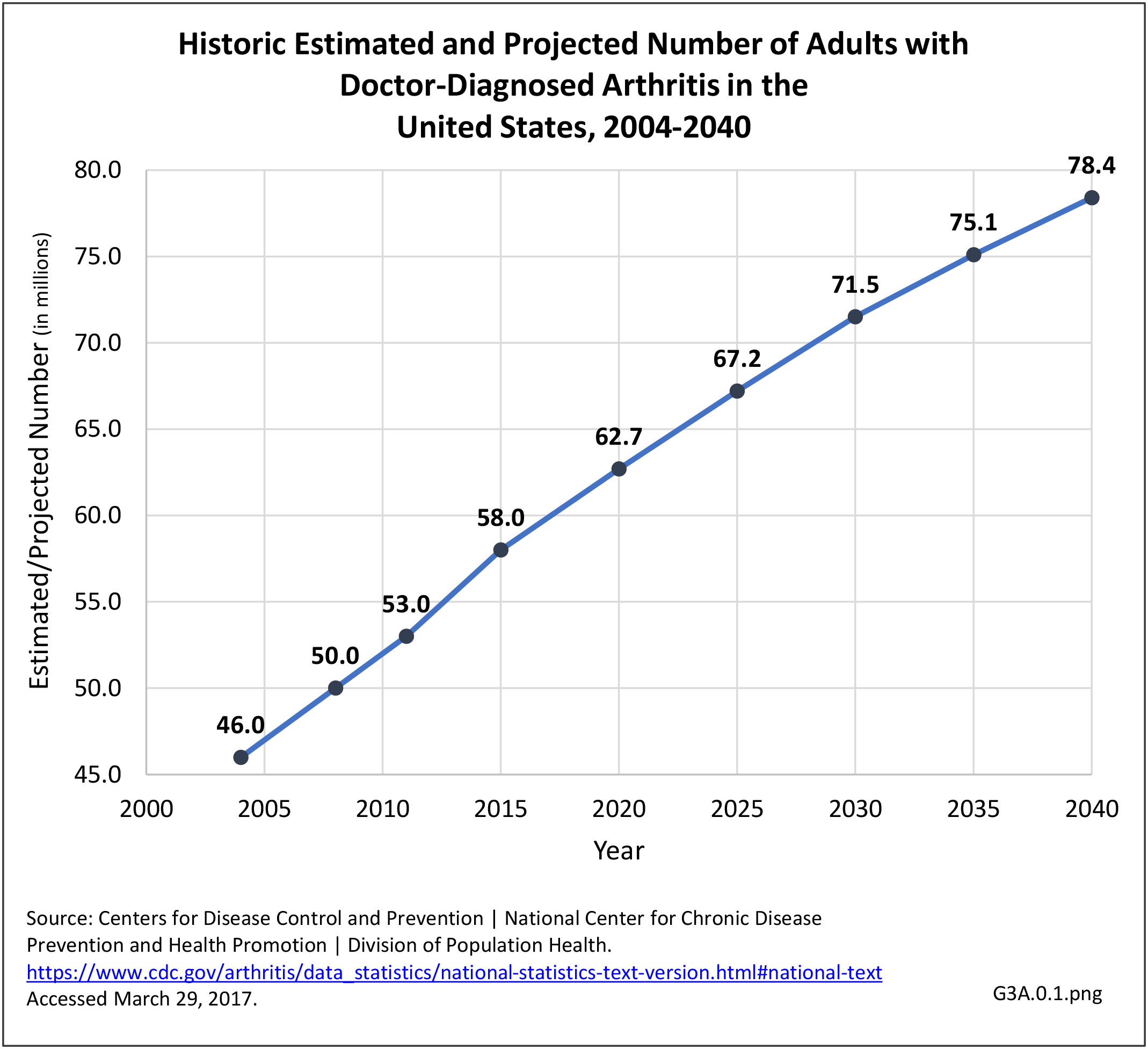
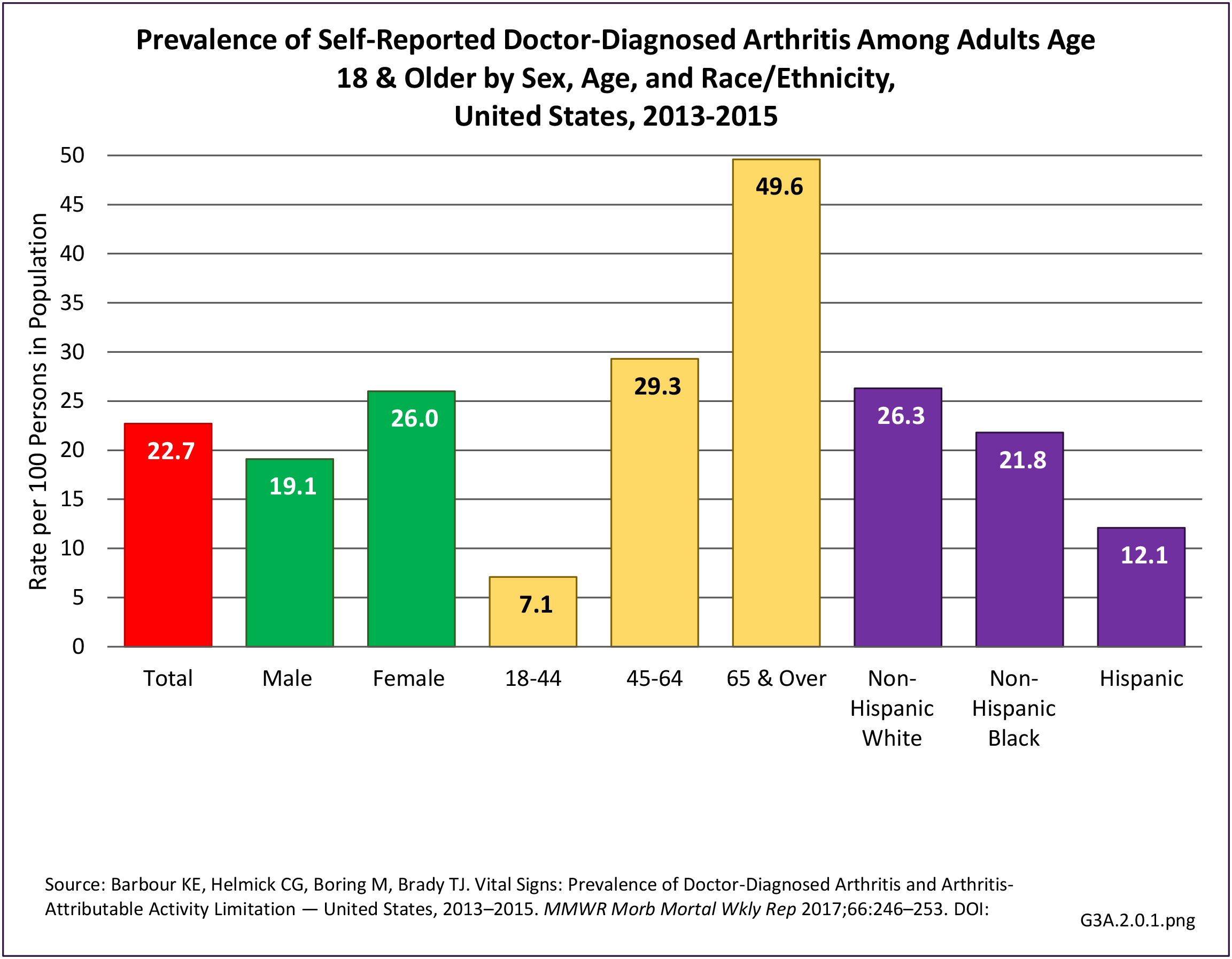
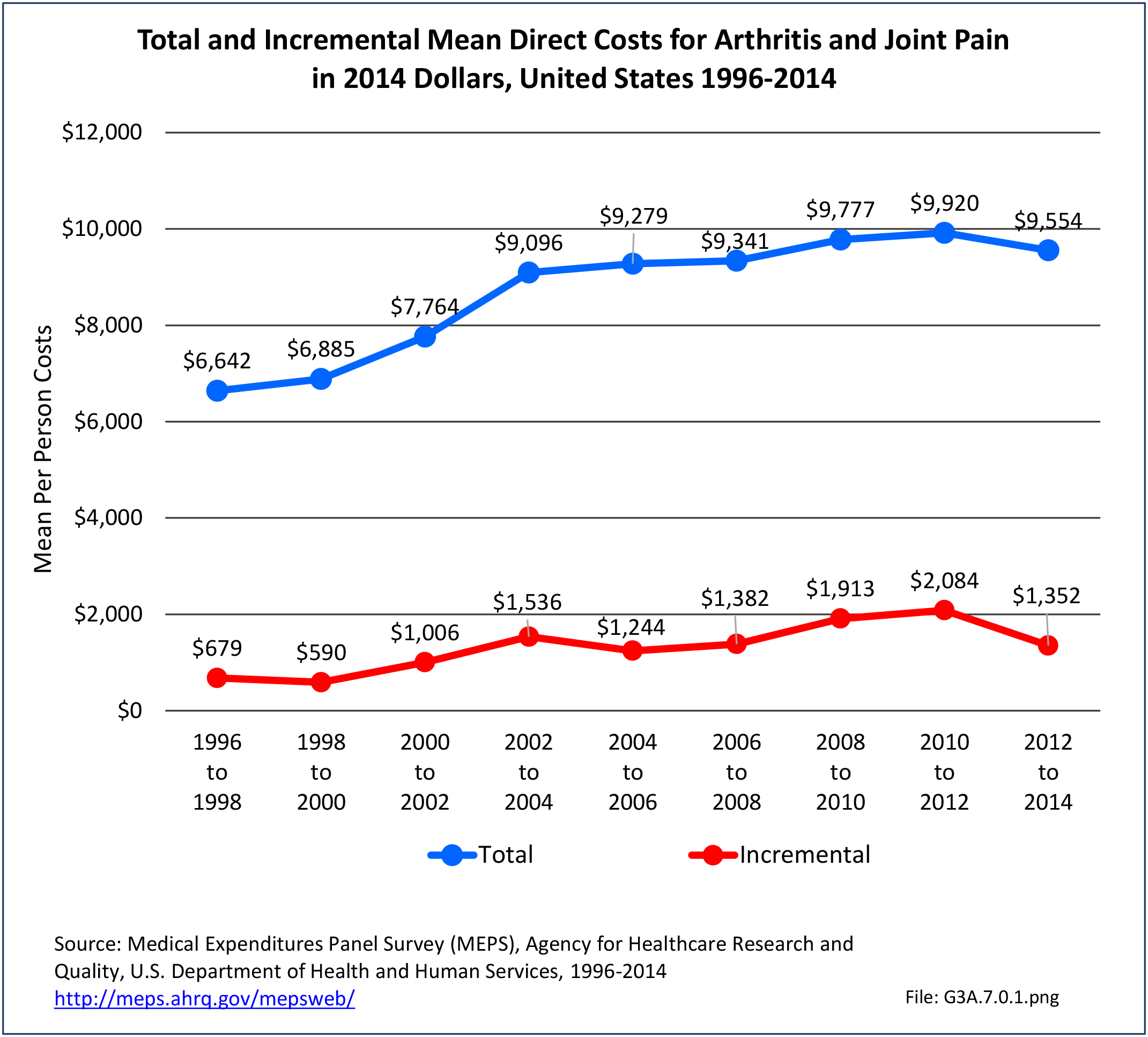
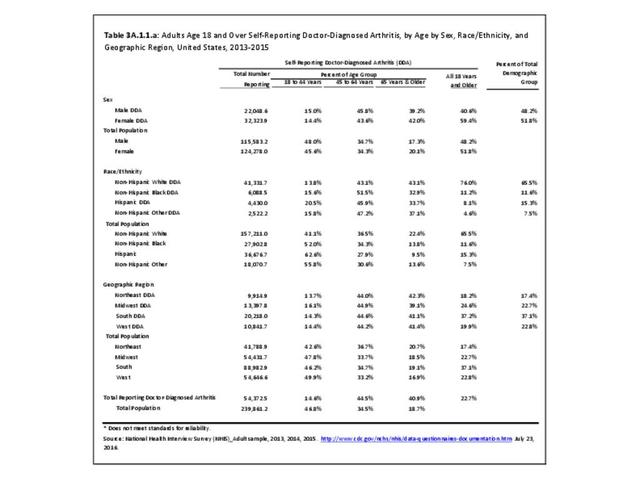
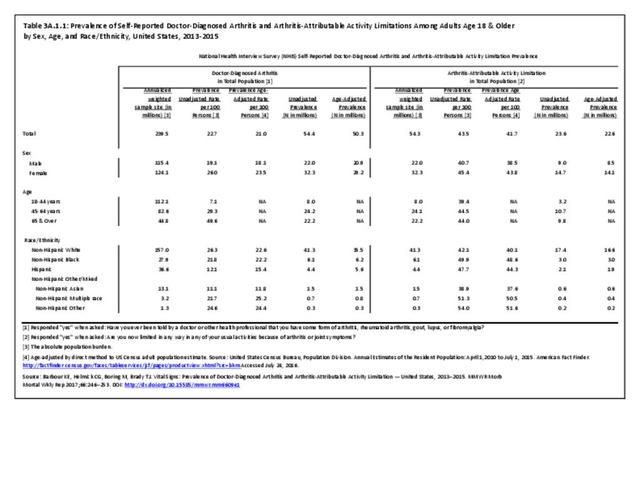
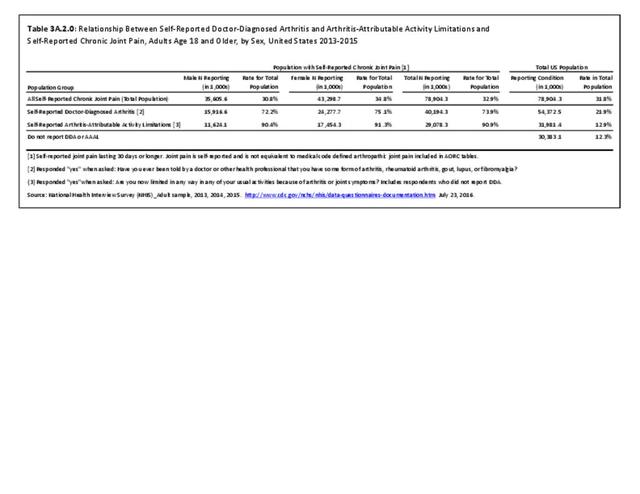
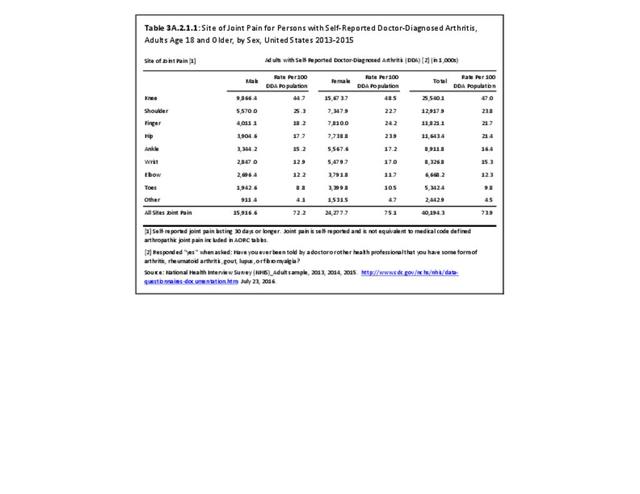
Research funding to develop and evaluate more effective clinical and public health interventions is relatively modest, given that arthritis is the most common cause of disability and is a large and growing problem, affecting 54.4 million adults now,2 and a projected 78 million by 2040.3 This is especially frustrating because even the evidence-based interventions we have now are not reaching the people who would benefit from them. Implementation research to translate effective interventions to clinical practice and/or community settings is needed.
Although most adults with doctor-diagnosed arthritis are younger than age 65 and in their working years, the effect of their arthritis on employment and work, and the effect of reasonable workplace accommodations, have not been explored in depth. There is a need for the development and demonstration of web-based or app-based interventions for education, physical activity and achieving a healthy weight. This is an urgent issue right now and will continue to be an urgent issue as an aging workforce keeps working beyond age 65, as is anticipated.
- 1. Office of Disease Prevention and Health Promotion. HealthyPeople.gov. http://www.healthypeople.gov/2020/data-search/Search-the-DData?&f[0]=field_topic_area%3A3507 Accessed October 24, 2018.
- 2. Barbour KE, Helmick CG, Boring M, Brady TJ. Vital signs: prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation — United States, 2013–2015. MMWR 2017;66:246–253. DOI: http://dx.doi.org/10.15585/mmwr.mm6609e1. Accessed July 31, 2017.
- 3. Hootman JM, Helmick CG, Barbour KE, et al. Updated projected prevalence of self-reported doctor-diagnosed arthritis and arthritis-attributable activity limitation among US adults, 2015-2040. Arthritis Rheumatol 2016:68(7):1582-1587.
Edition:
- Fourth Edition