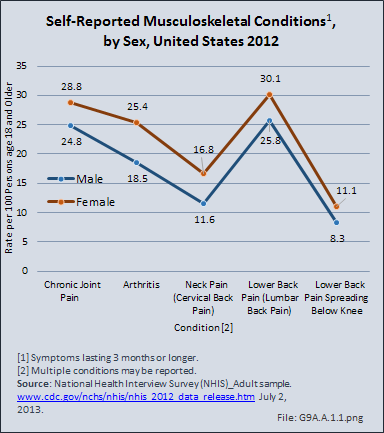
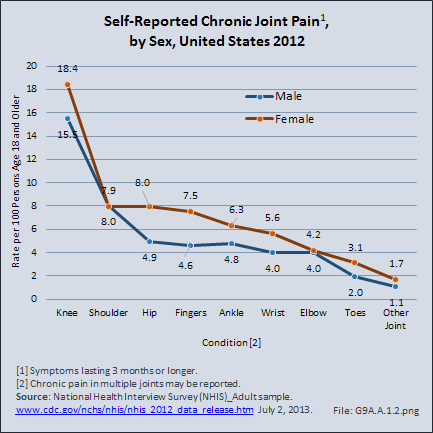
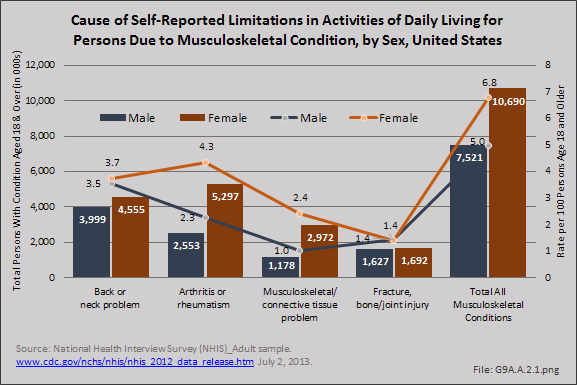
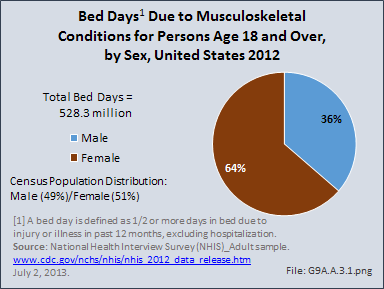
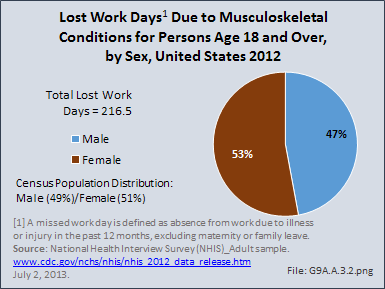
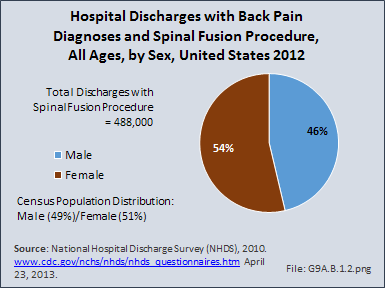
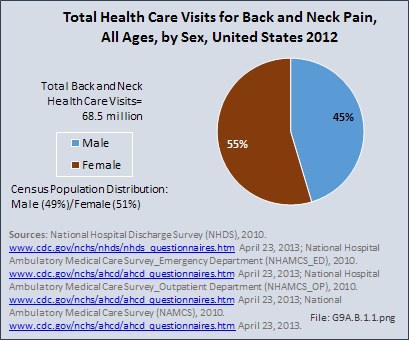
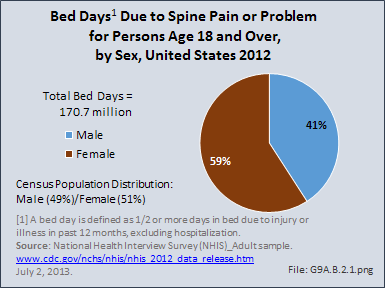
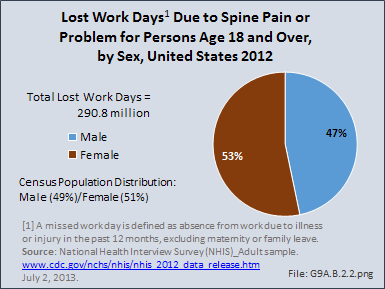
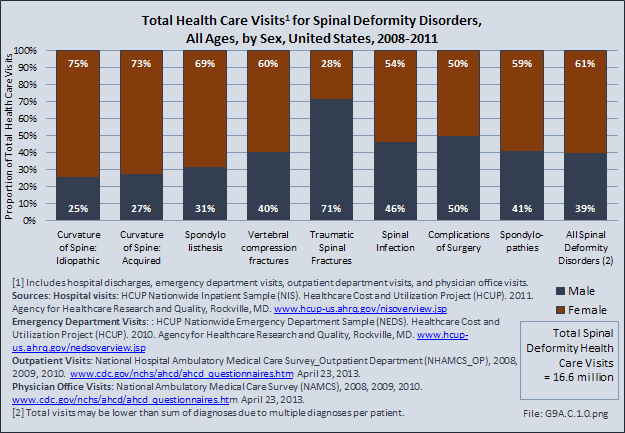
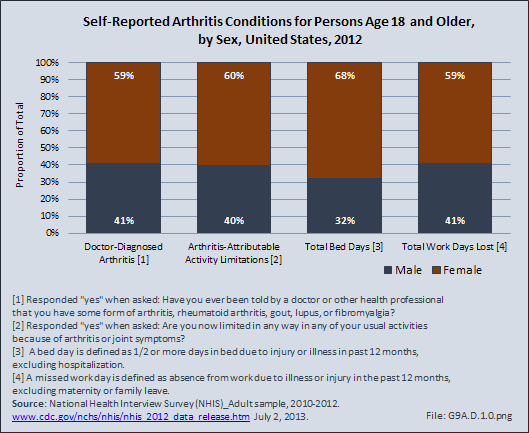
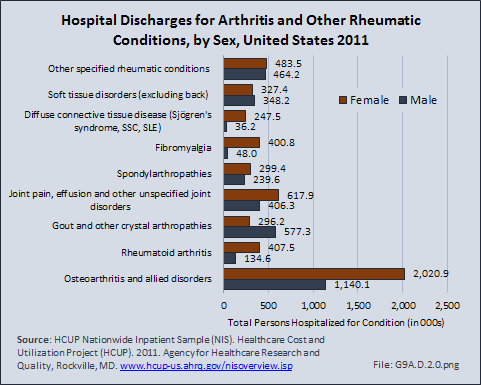
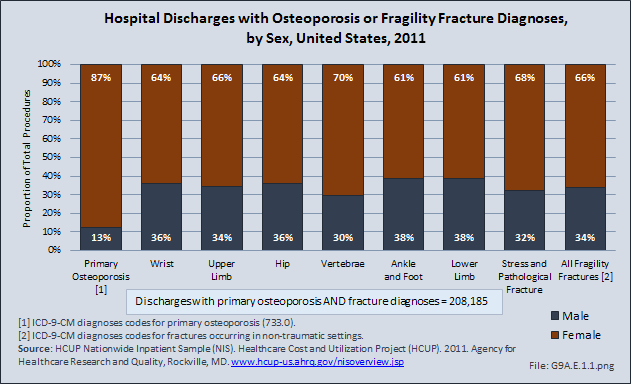
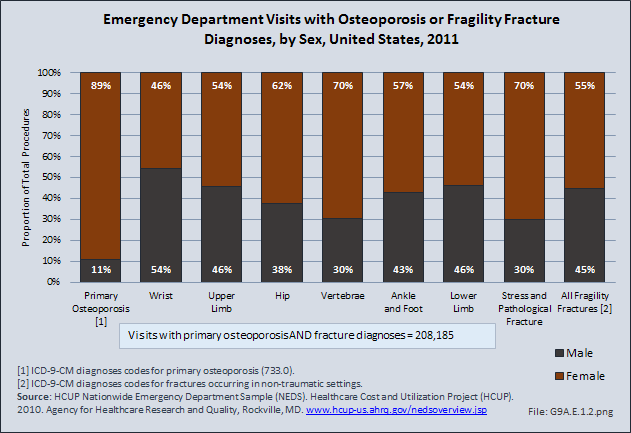
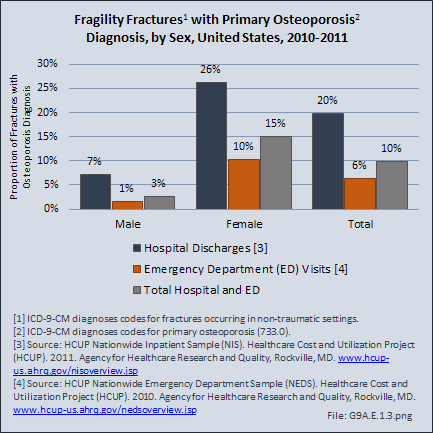
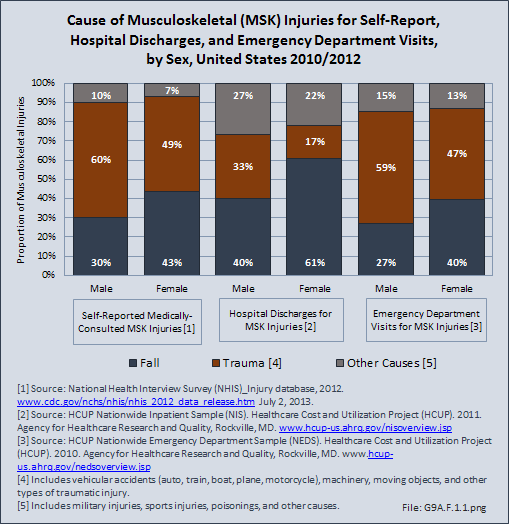
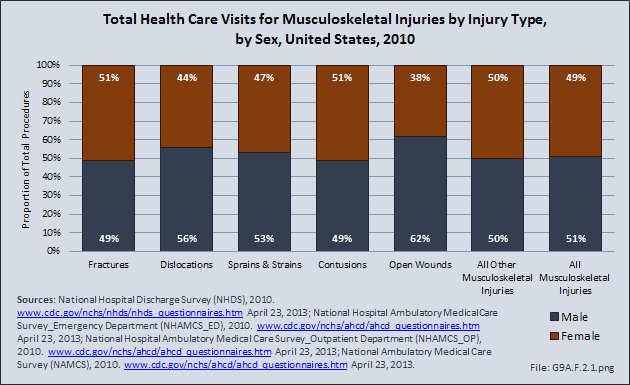
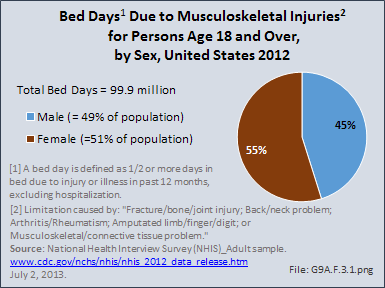
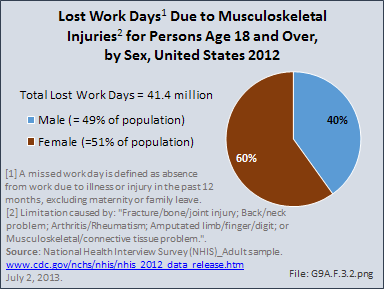
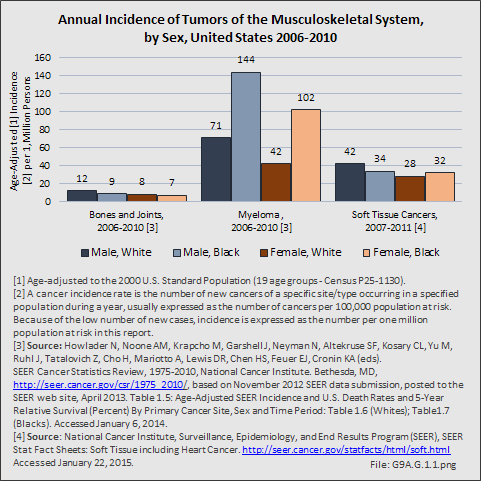
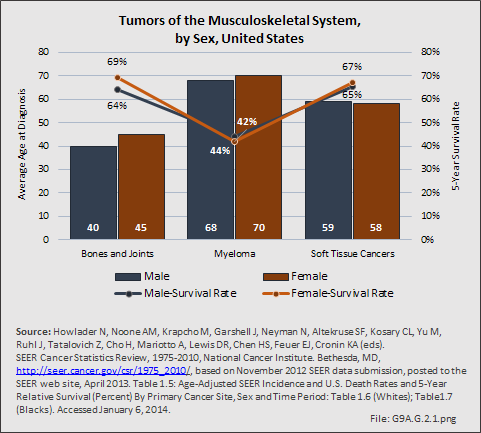
The relative impacts of sex and gender on etiology and responses to treatment need to be defined for all musculoskeletal conditions. Evidence at this point indicates that women experience musculoskeletal conditions in higher numbers than men do for all conditions except traumatic injuries and cancers of the musculoskeletal system. The smaller differences such as those found in musculoskeletal injuries and spine conditions are moderate. Differences in incidence for some conditions, such as osteoporosis, spinal deformity, and arthritis, are sufficient to warrant exploration into reasons why these differences occur.
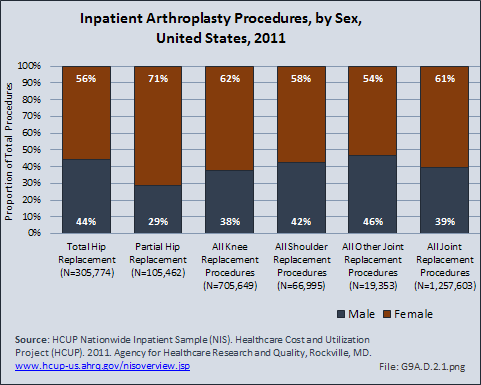
The impact of sex on musculoskeletal conditions may reflect differences in levels of or response to sex hormones. However, the relative impact of these hormones between the sexes and during different phases of the menstrual cycle have not been clearly elucidated, and although it is likely sex hormones impact on most, if not all, musculoskeletal conditions, additional factors need to be investigated. As the Institute of Medicine says, “every cell has a sex,”1 and these cell-based differences reflect much more than response to sex hormones. Identification of sex-based factors related to causes of disease will be key to prevention. Sex-based differences in responses to treatment may indicate a need to tailor treatment options to individual patients. The latter is exemplified by the significant differences between the sexes in outcome of metal-on-metal hip arthroplasty,2 which may also be influenced by sex-based genetic differences.3 In addition, the impact of gender needs to be clarified. Although prevention and treatment options are available, if there is not awareness that these conditions occur in all patients, and patients of either gender are less able or not encouraged to access these resources, the outcome of their treatment is less likely to be delayed, impacting function, and raising the societal costs of these conditions.
- 1. Institute of Medicine. Exploring the Biological Contributions to Human Health: Does Sex Matter? Washington, DC, The National Academy Press, 2001, pp. 24-44. Available at http://www.nap.edu/catalog/10028/exploring-the-biological-contributions-to-human-health-does-sex-matter. Accessed March 11, 2011. ISBN: 978-0-309-07281-6.
- 2. Latteier MJ, Berend KR, Lombardi AV Jr, et al: Gender is a significant factor for failure of metal-on-metal total hip arthroplasty. J Arthroplasty 2011;26(6):19-23. doi: 10.1016/j.arth.2011.04.012. Epub 2011 Jun 8.
- 3. Bachmann HS, Hanenkamp S, Komacki B, et al. Gender-dependent association of GNSS1 T393C polymorphism with early aseptic loosening after total hip arthroplasty. J Orthop Res 2008 Dec;26(12):1562-1568. doi: 10.1002/jor.20699.
Edition:
- 2014

 Download as CSV
Download as CSV