Zoek je naar onbegrensde vrijheid en gemak bij online casino’s zonder CRUKS? Met internationale aanbieders profiteer je van snelle stortingen, flinke bonussen en meer privacy. 🎰
Heb je zin om te spelen bij een casino zonder CRUKS en wil je weten welke aanbieders écht de moeite waard zijn? In onze lijst hieronder zie je wie er hoog scoren op spelaanbod, betrouwbaarheid en gebruikerservaring. Je krijgt meer privacy, vaak hogere bonussen en kunt meestal sneller je winst opnemen. Kies jouw favoriet en duik in een wereld van onvervalst speelplezier!
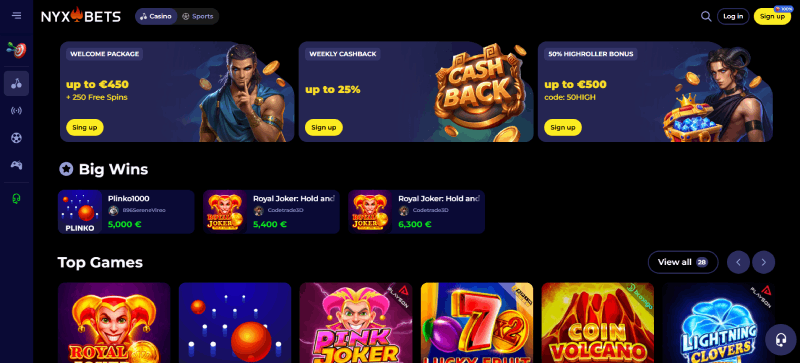
| 🥇 NYXbets | Beste casino zonder CRUKS in Nederland |
| 🥈 BinoBet | Beste mobiele casino zonder CRUKS |
| 🥉 TrueLuck | Snelste casino uitbetalingen zonder CRUKS |
| ⭐ Booms.Bet | Beste live casino zonder CRUKS |
| ⭐ GXbet | No-CRUKS casino met topbeloningen voor spelers |
Ben je klaar om zorgeloos te gokken, zónder CRUKS? In ons overzicht voor 2025 vind je aanbieders met ruime bonussen, vlotte uitbetalingen en maximale privacy. Zo geniet je elke sessie van optimale vrijheid en kans op mooie winsten.
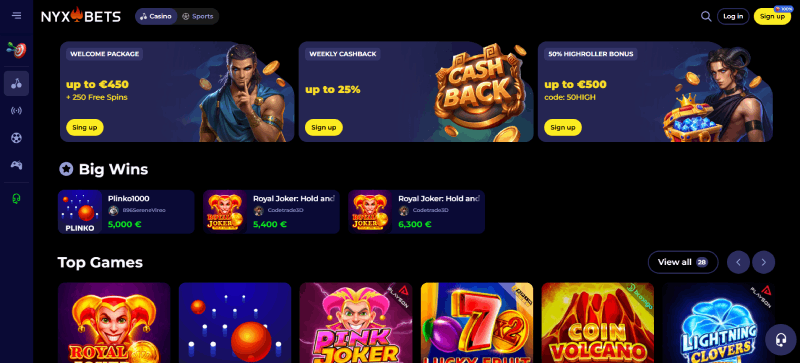
| ⚡ Uitbetaling | 0-1 uur |
| 🎁 Online casino bonus | €450 en 250 Free Spins + 25% Cashback |
| 🔓 Zonder CRUKS? | ✅ |
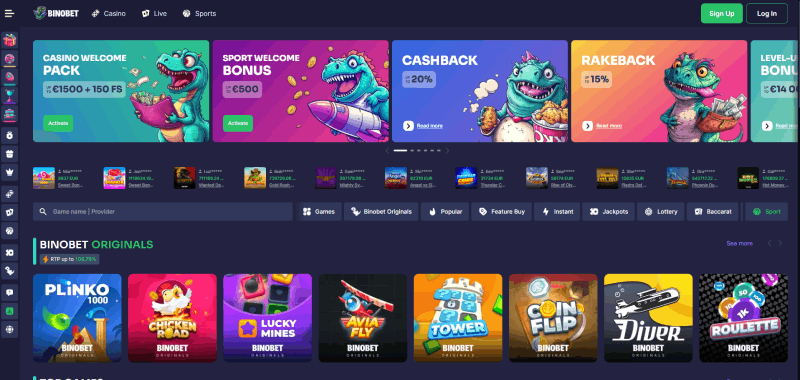
| ⚡ Uitbetaling | 0-2 uur |
| 🎁 Online casino bonus | €1500 en 150 Free Spins + tot 20% Cashback & 15% Rakeback |
| 🔓 Zonder CRUKS? | ✅ |
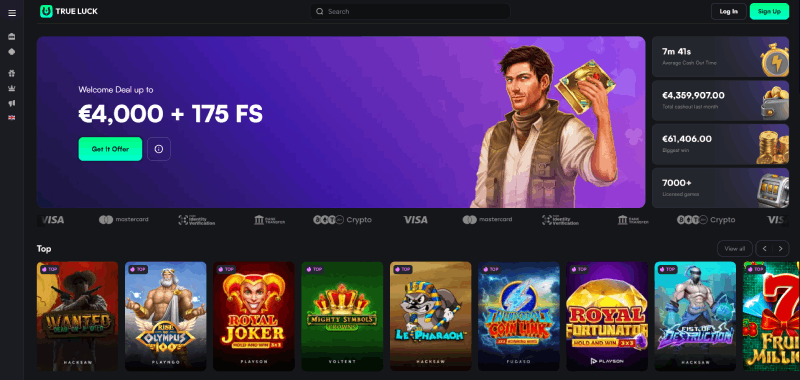
| ⚡ Uitbetaling | 0-2 uur |
| 🎁 Online casino bonus | €4000 en 175 Free Spins + tot 15% Cashback |
| 🔓 Zonder CRUKS? | ✅ |
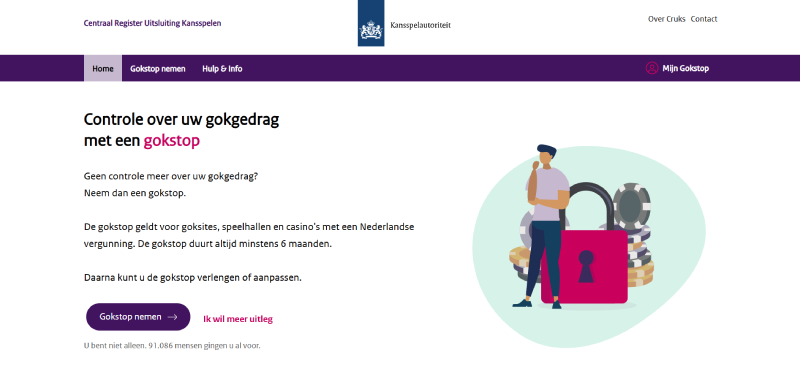
CRUKS staat voor het Centraal Register Uitsluiting Kansspelen, een systeem dat door de Nederlandse kansspelautoriteit is opgezet. Het geldt voor binnenlandse casino’s met een KSA-vergunning en dient om spelers te beschermen die te veel risico lopen op gokverslaving.
Zodra je bent opgenomen in CRUKS, mag je niet meer spelen in casino’s met een Nederlandse licentie. De bedoeling is dat kwetsbare spelers extra begeleiding en pauze krijgen. Veel mensen kiezen echter voor casino’s zonder CRUKS om hun speelvrijheid en privacy te behouden.
Bij casino’s zonder CRUKS kun je sneller registreren en direct spelen, zonder dat je beperkt wordt door een nationale uitsluiting.
Spelen bij een casino zonder CRUKS betekent dat je geen verplichte inschrijving bij het Nederlandse register hoeft te doorlopen. Dit geeft je meer mogelijkheden om je eigen keuzes te maken.
Je hoeft geen documenten of registraties van CRUKS te doorlopen, zodat je direct kunt beginnen met spelen. Deze vrijheid wordt gewaardeerd door spelers die liever zelf hun gokgedrag beheersen in plaats van zich te houden aan strikte regels.
Een casino zonder CRUKS vraagt meestal minder gevoelige informatie tijdens het aanmeldproces. Daardoor behouden veel spelers graag de controle over hun gegevens, wat bijdraagt aan een veilige en anonieme speelervaring die je niet snel bij Nederlandse sites vindt.
Doordat er geen verplichte CRUKS-check is, ervaar je minder restricties tijdens het inzetten en ben je vrijer in je speellimieten. Dit kan bijvoorbeeld prettig zijn voor ervaren gokkers die graag op hun eigen voorwaarden spelen en hun eigen risico bepalen.
Bij casino’s zonder CRUKS verloopt het registratieproces doorgaans snel: je vult basisinformatie in, kiest een wachtwoord en kunt vrijwel direct beginnen. Deze straightforward aanpak is ideaal als je geen zin hebt in ellenlange formulieren of ID-checks.
Veel casino’s zonder CRUKS bezitten een licentie uit landen zoals Malta, Curaçao of Kahnawake. Ondanks dat deze vergunningen niet door de Nederlandse autoriteit worden verstrekt, hanteren ze vaak strenge regels rond verantwoord spelen, eerlijke games en beveiliging van betalingen.
Je vindt hier betaalmethoden die in Nederland misschien nog niet zo bekend zijn, maar wel snel en efficiënt werken. Voorbeelden zijn cryptobetalingen, alternatieve e-wallets of internationale overschrijvingen die je bij veel binnenlandse aanbieders niet zomaar tegenkomt.
Door de minder strikte regelgeving in het buitenland, bieden casino’s zonder CRUKS vaak gul mogelijke bonussen. Denk aan hoge welkomstpakketten, regelmatige toernooien en exclusieve acties die anders in Nederland wellicht niet worden toegestaan door de Kansspelautoriteit.
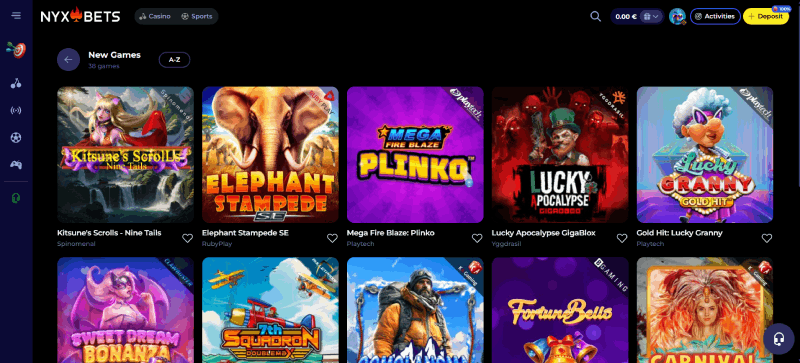
In deze casino’s stuit je vaak op gokspellen van ontwikkelaars die op de Nederlandse markt niet actief zijn. Zo profiteer je van een unieke mix van klassieke slots, moderne videoslots, live tafels en innovatieve spelconcepten die je horizon verbreden.
Veel spelers vragen zich af of een casino zonder CRUKS echt zo verschillend is van een Nederlands casino mét CRUKS. In de kern kun je dezelfde soorten spellen spelen, maar de grote verschillen zitten ‘m in privacy, bonusvoorwaarden en registratievereisten.
| Kenmerk | Casino met CRUKS | Casino zonder CRUKS |
|---|---|---|
| Licentie | Nederlandse KSA-vergunning | Malta, Curaçao, Kahnawake, enzovoort |
| Betaalmethoden | Beperkt door NL-regels | Ruimere opties, ook crypto of buitenlandse |
| Spelaanbod | Voornamelijk bekende providers | Grotere variatie, internationale ontwikkelaars |
| Bonussen | Vaak strak gereguleerd | Hoger, meer flexibiliteit |
| CRUKS-registratie | Verplicht (indien opgenomen) | Niet van toepassing |
| Uitbetaalsnelheid | Kan soms langer duren | Regelmatig razendsnel |
| Restricties | Meestal strengere limieten | Vrijer, speler beslist zelf |
Wanneer je wil genieten van vrij gokken zonder CRUKS, kun je eenvoudig kiezen voor een aanbieder met een buitenlandse licentie. Het proces van aanmelding tot uitbetaling verloopt sneller dan bij Nederlandse casino’s. Zo kun je in slechts enkele stappen je account activeren en beginnen met spelen.
We raden je aan om eerst onze top lijst van beste casino’s zonder CRUKS te bekijken. Vanuit onze ervaring doen deze aanbieders er alles aan om je een vlotte registratie en aantrekkelijke promoties te geven. Selecteer je favoriet en ga door naar het volgende stappenplan voor je eerste storting.
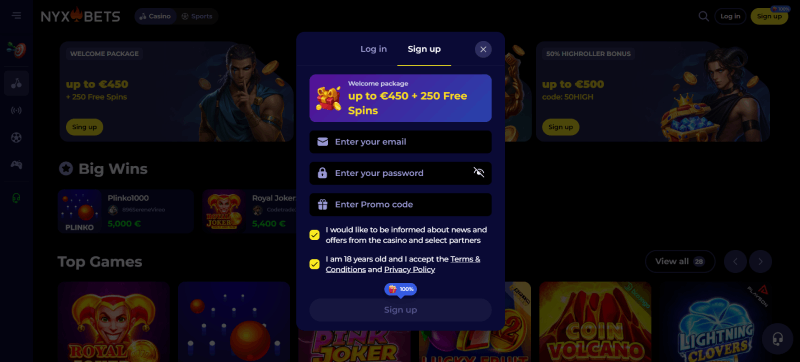
Klik op “Registreren” of “Maak een account aan” en vul de nodige gegevens in. Meestal vraag je alleen om je naam, e-mailadres en een wachtwoord. Je rondt dit in een paar minuten af en kunt vervolgens je accountactivering via een bevestigingsmail afronden.
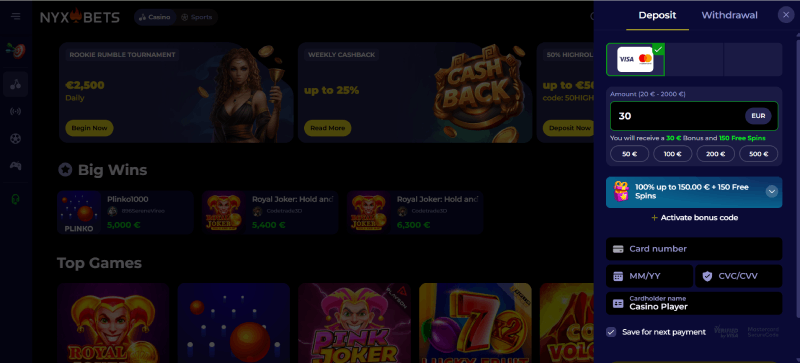
Ga naar de kassier-sectie en kies een betaalmethode die bij je past. Bij casino’s zonder CRUKS kun je vaak terecht met internationale e-wallets, creditcards, bankoverschrijvingen of zelfs cryptobetalingen. Stort je gewenste bedrag, zorg dat je saldo is aangevuld en ga naar de spellenlobby om te beginnen spelen.
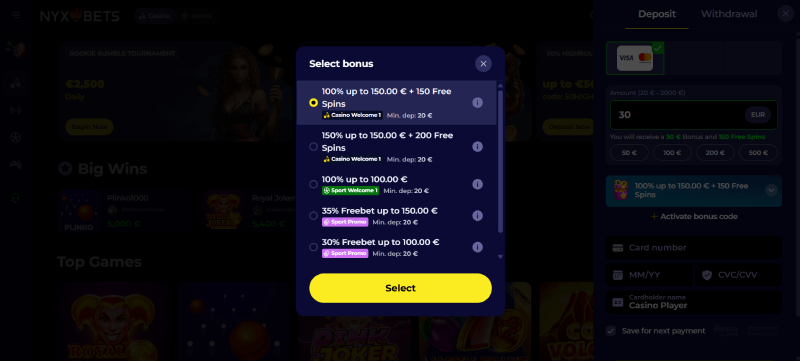
Om je speeltijd extra spannend te maken, kun je gebruikmaken van de welkomstbonus. Dit is meestal een combinatie van extra speeltegoed en soms free spins. Check de bonusvoorwaarden en activeer je aanbieding door een code in te voeren of door een vinkje aan te zetten tijdens je storting.
Nu je saldo op orde is, kun je meteen je favoriete spellen openen. Geniet van slots, live tafelspellen, bingo of crash games en test je geluk. Kom je in de prijzen? Dan kun je eenvoudig je winst laten uitbetalen op dezelfde betaalmethode die je hebt gebruikt.
Speel je bij een casino zonder CRUKS, dan krijg je een wereld aan vrijheid en gemak, maar er zijn ook aandachtspunten. Hieronder vind je de belangrijkste pluspunten en enkele minpunten op een rij. Wees je hiervan bewust om zorgeloos te genieten.

Niet alle casino’s zonder CRUKS zijn onbetrouwbaar. Sterker nog, veel van deze aanbieders hebben een vergunning uit Malta, Curaçao, Kahnawake of andere betrouwbare jurisdicties. Deze instanties stellen ook strikte eisen op het gebied van spelersbescherming, eerlijke software en de afhandeling van financiële transacties.
Hoewel ze niet aan de Nederlandse KSA-regels voldoen, zijn de wettelijke kaders vaak stevig genoeg om spelers goed te beschermen. Dit betekent dat je alsnog met een gerust hart kunt spelen, zolang je kiest voor gerenommeerde partijen die hun licentie serieus nemen.
Kies altijd een casino met een zichtbare en controleerbare vergunning om veilig en verantwoord te spelen.
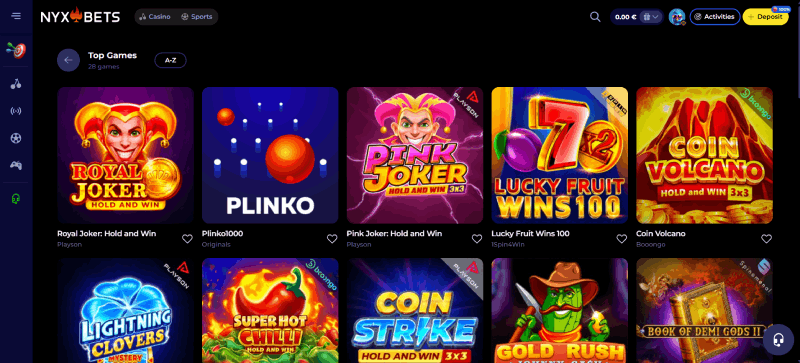
Een casino zonder CRUKS geeft je meestal toegang tot een brede waaier aan spellen, van klassieke fruitautomaten tot moderne live games. Hierdoor is de kans groter dat je iets vindt dat perfect bij je smaak aansluit.
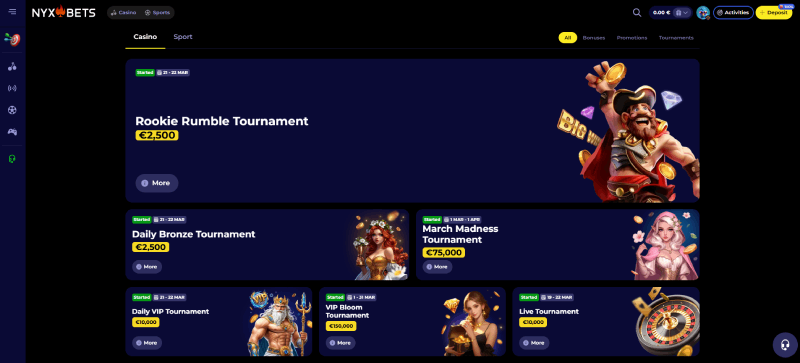
Bij een casino zonder CRUKS kom je vaak promoties tegen die in Nederland aan banden zijn gelegd. Denk aan royale welkomstpakketten die je speeltegoed verdubbelen, free spins op populaire slots, cashback-acties voor trouwe leden of zelfs toernooien met cashprijzen.
Deze bonussen zijn bedoeld om je interesse vast te houden en je bankroll te vergroten. Let wel op de voorwaarden, zoals inzetvereisten, geldigheidsduur en maximale winstlimieten. Zo haal je optimaal voordeel uit de extra aanbiedingen die buitenlandse casino’s te bieden hebben, zonder verrassingen achteraf.
Casino’s zonder CRUKS bieden vaak hogere bonussen en meer variatie dan Nederlandse aanbieders.
Zonder CRUKS heb je doorgaans meer keuze om te storten en uit te betalen. Naast de bekende opties als creditcards en e-wallets, bieden buitenlandse casino’s vaak ook crypto-betalingen of minder gangbare diensten uit andere landen. Dit geeft je de kans om alternatieve, mogelijk snellere methoden te gebruiken.
Omdat de lokale regelgeving minder streng is dan in Nederland, kunnen deze casino’s een breder palet aan financiële diensten aanbieden. Hierdoor geniet je van een vlotte afhandeling van transacties en kun je direct door naar de spellen, zonder ingewikkelde controles.
Crypto-betalingen zijn snel en vaak zonder extra kosten, ideaal voor spelers die anoniem willen blijven.
Bij de meeste casino’s zonder CRUKS kun je niet direct met iDEAL betalen, omdat ze geen Nederlandse licentie hebben. Toch is hier een handige omweg voor. Via diensten als Volt, Yaspa of Brite kun je betalingen doen die vergelijkbaar zijn met iDEAL, of zelfs met iDEAL worden gefund. Hierdoor is het alsnog mogelijk om binnen een paar muisklikken saldo te storten en met je favoriete betaalmethode aan de slag te gaan.
Spelen zonder CRUKS betekent niet dat je roekeloos aan de slag moet gaan. Hier zijn vijf tips om op een gezonde, prettige manier om te gaan met online gokken bij buitenlandse casino’s.
Speel je bij een casino zonder CRUKS, dan kies je voor meer vrijheid, aantrekkelijke bonussen en uitgebreide betaalopties—zonder de strikte Nederlandse controles. Dit geeft je de kans om op je eigen tempo te spelen en sneller uit te laten betalen.
Ook het spelaanbod is vaak groter en internationaal georiënteerd, wat zorgt voor extra variatie. Wil je dus zorgeloos genieten van online entertainment en optimale privacy? Ontdek onze aanbevolen aanbieders en vind jouw perfecte gokplek!
Een casino zonder CRUKS is een online aanbieder die geen gebruikmaakt van het Nederlandse Centraal Register Uitsluiting Kansspelen. Je kunt hier spelen zonder Nederlandse licentiecheck en verplichte inschrijvingen. Hierdoor ervaar je meer vrijheid en privacy, maar heb je ook minder bescherming vanuit de Nederlandse overheid.
Ja, casino’s zonder CRUKS kunnen gewoon legaal opereren, maar niet met een Nederlandse vergunning. Deze sites beschikken meestal over licenties uit landen als Malta, Curaçao of Kahnawake. Hoewel ze niet door de KSA gereguleerd worden, zijn veel van deze aanbieders nog steeds betrouwbaar en voldoen ze aan strenge eisen.
Uitschrijven uit CRUKS gebeurt via de officiële website van de Kansspelautoriteit of met hulp van klantenservice in Nederlandse casino’s. Zodra je bent uitgeschreven, kun je bij deze binnenlandse aanbieders weer inloggen. Wil je echter helemaal niet in CRUKS terechtkomen, dan kies je voor casino’s zonder Nederlandse licentie.
Kijk allereerst of er een gerenommeerde buitenlandse licentie is, zoals die van de Malta Gaming Authority of Curaçao eGaming. Lees ervaringen van andere spelers en check onze top 3-aanraders. Controleer ook de beveiliging van de website, het spelaanbod en de snelheid van uitbetalingen.
Het grootste voordeel is de toegenomen vrijheid, zonder verplichte controles of registratie in het Nederlandse systeem. Bovendien bieden casino’s zonder CRUKS vaak hogere bonussen, vlotte betaalmethoden en een breder spelaanbod. Zo ervaar je meer flexibiliteit en mogelijkheden dan bij strikt gereguleerde Nederlandse online casino’s.