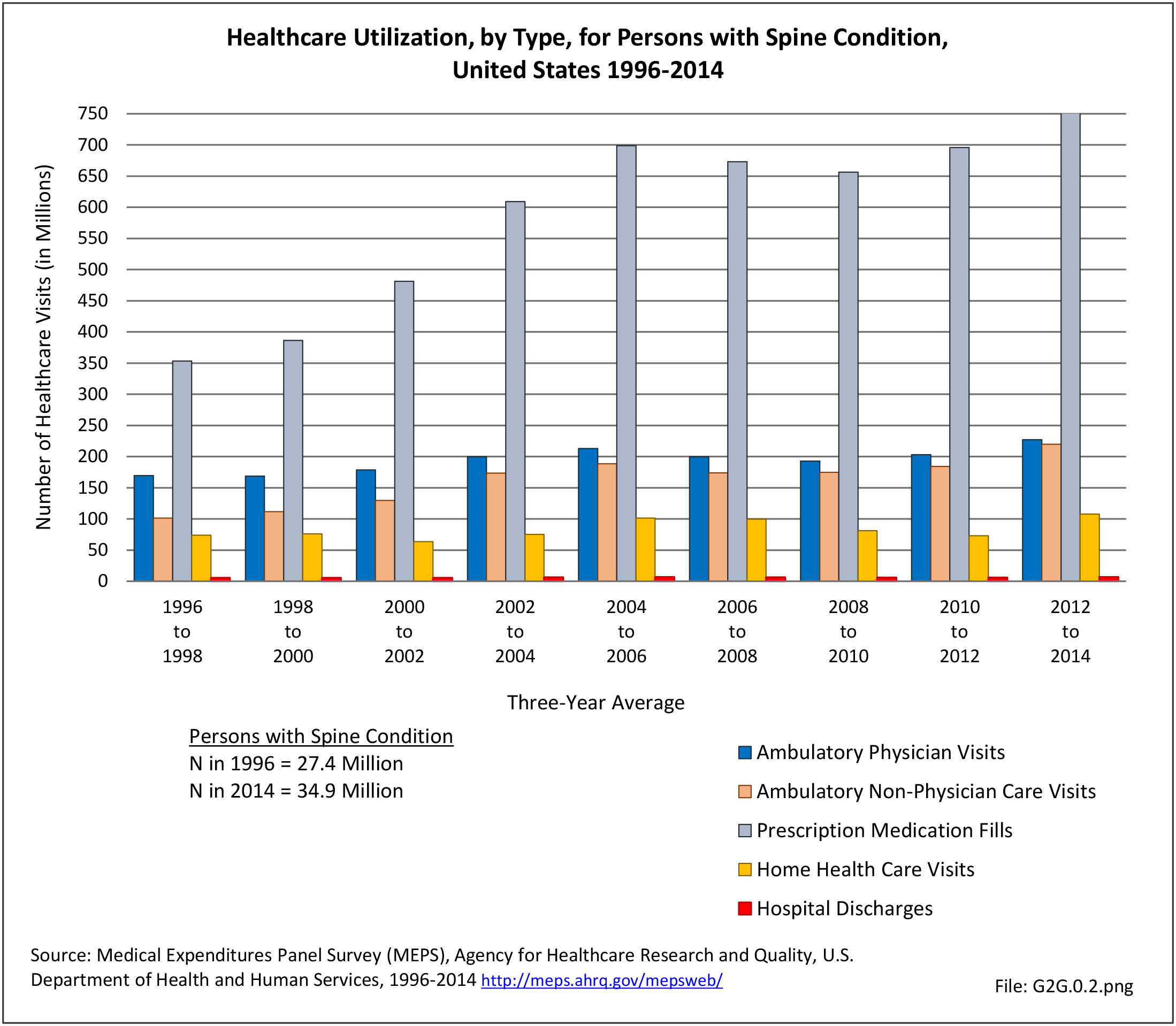
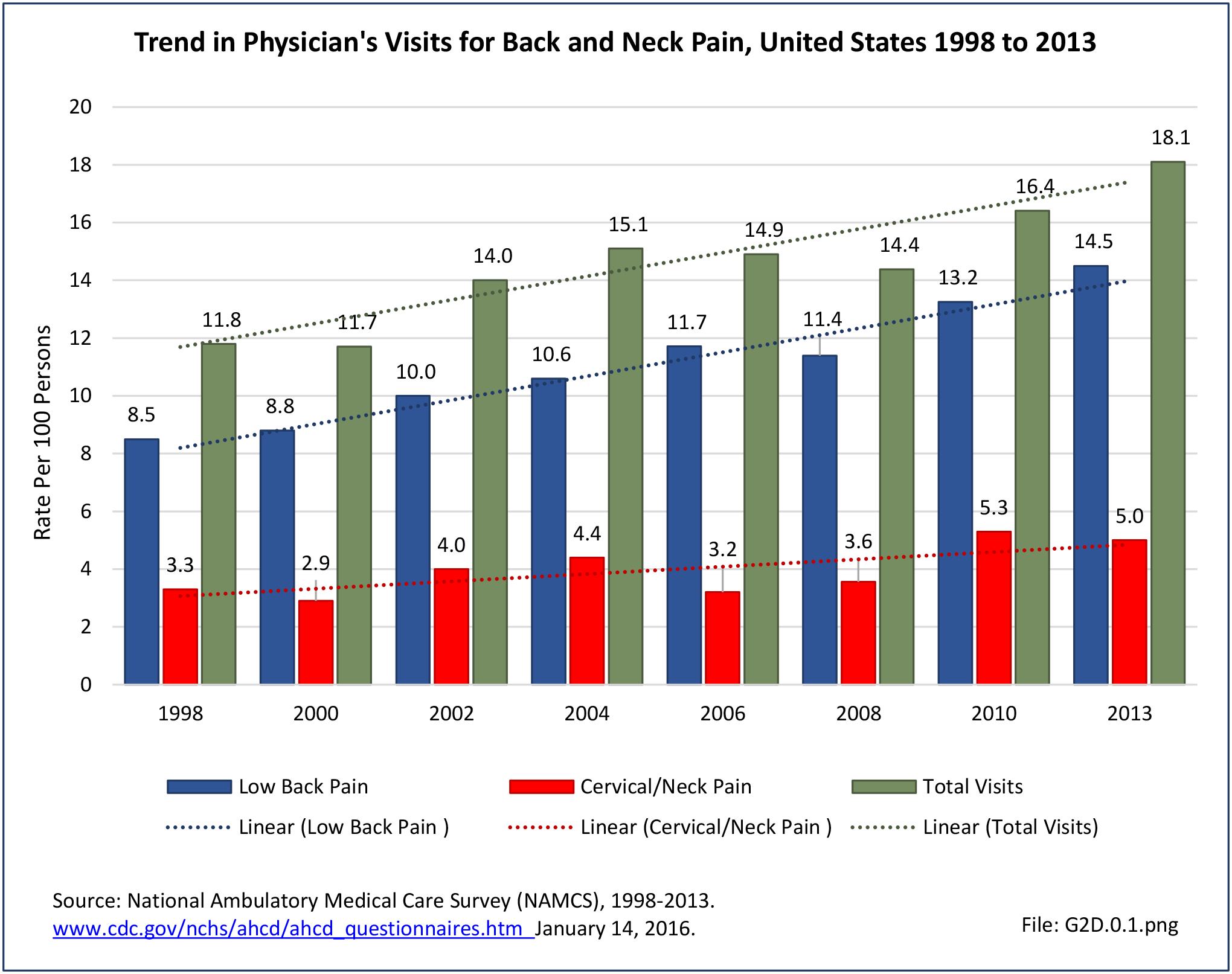
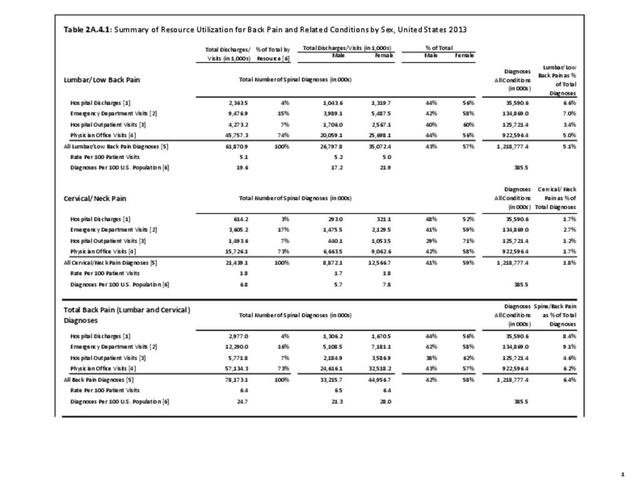
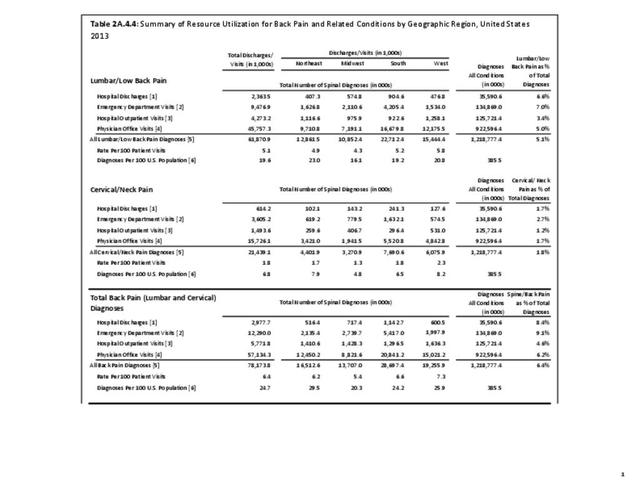
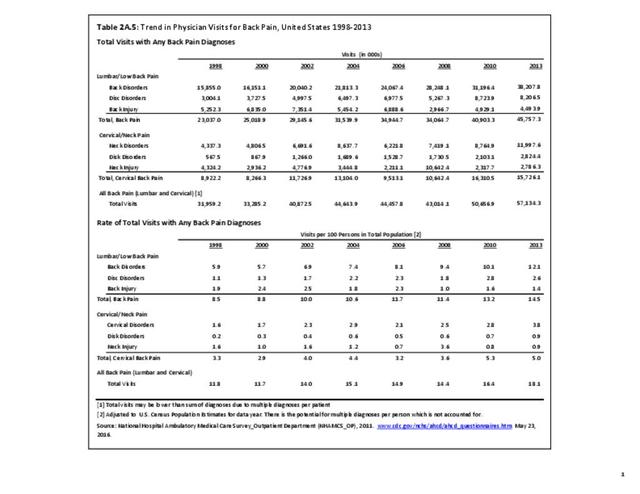
Lumbar/low back pain and cervical/neck pain are among the most common medical conditions requiring medical care and affecting an individual’s ability to work and manage the daily activities of life. Back pain is the most common physical condition for which patients visit their doctor. In any given year, between 12% and 14% of the United States adult population age 18 and okder visit their physician with complaints of back pain. The number of physician visits has increased steadily over the years. In 2013, more than 57.1 million patients visited a physician with a complaint of back pain, compared to 50.6 million in 2010. (Reference Table 2A.5 PDF CSV) In addition, an unknown number of patients visit a chiropractor or physical therapist for these complaints.
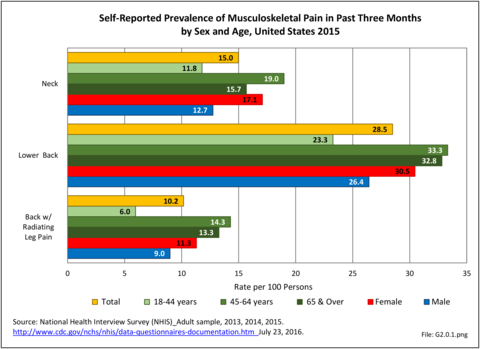
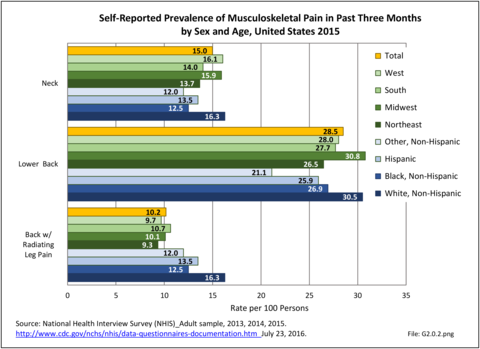
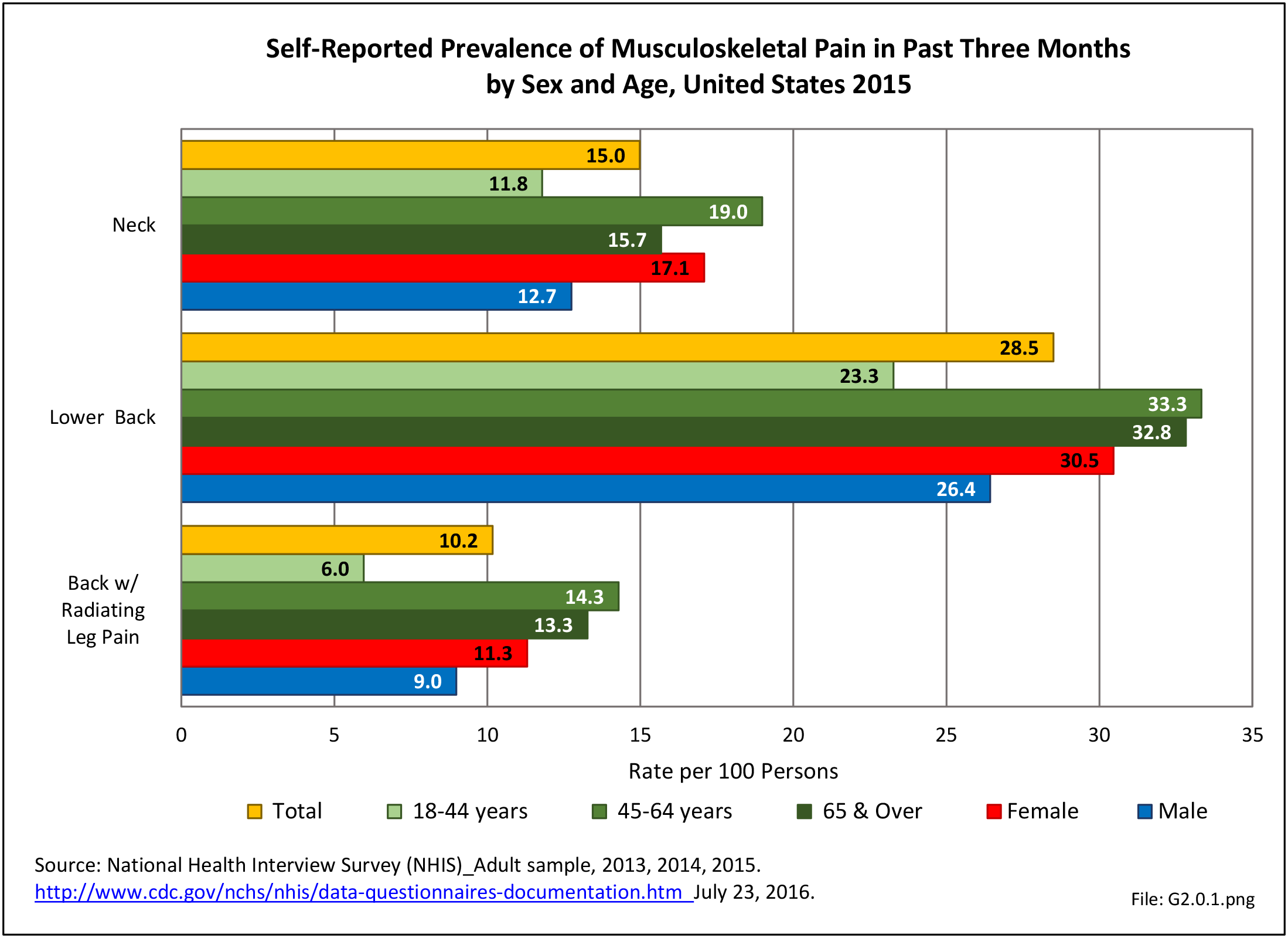
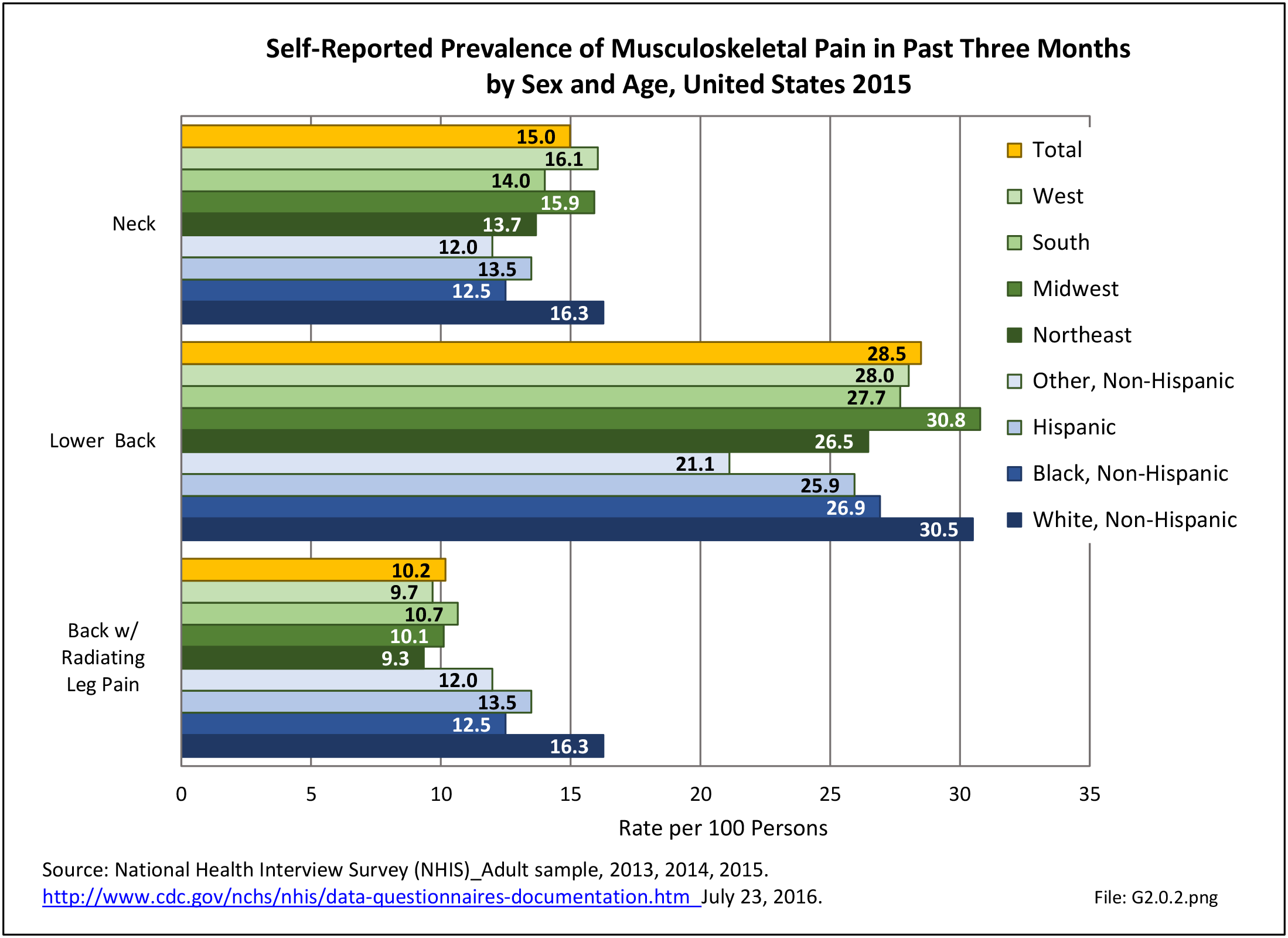
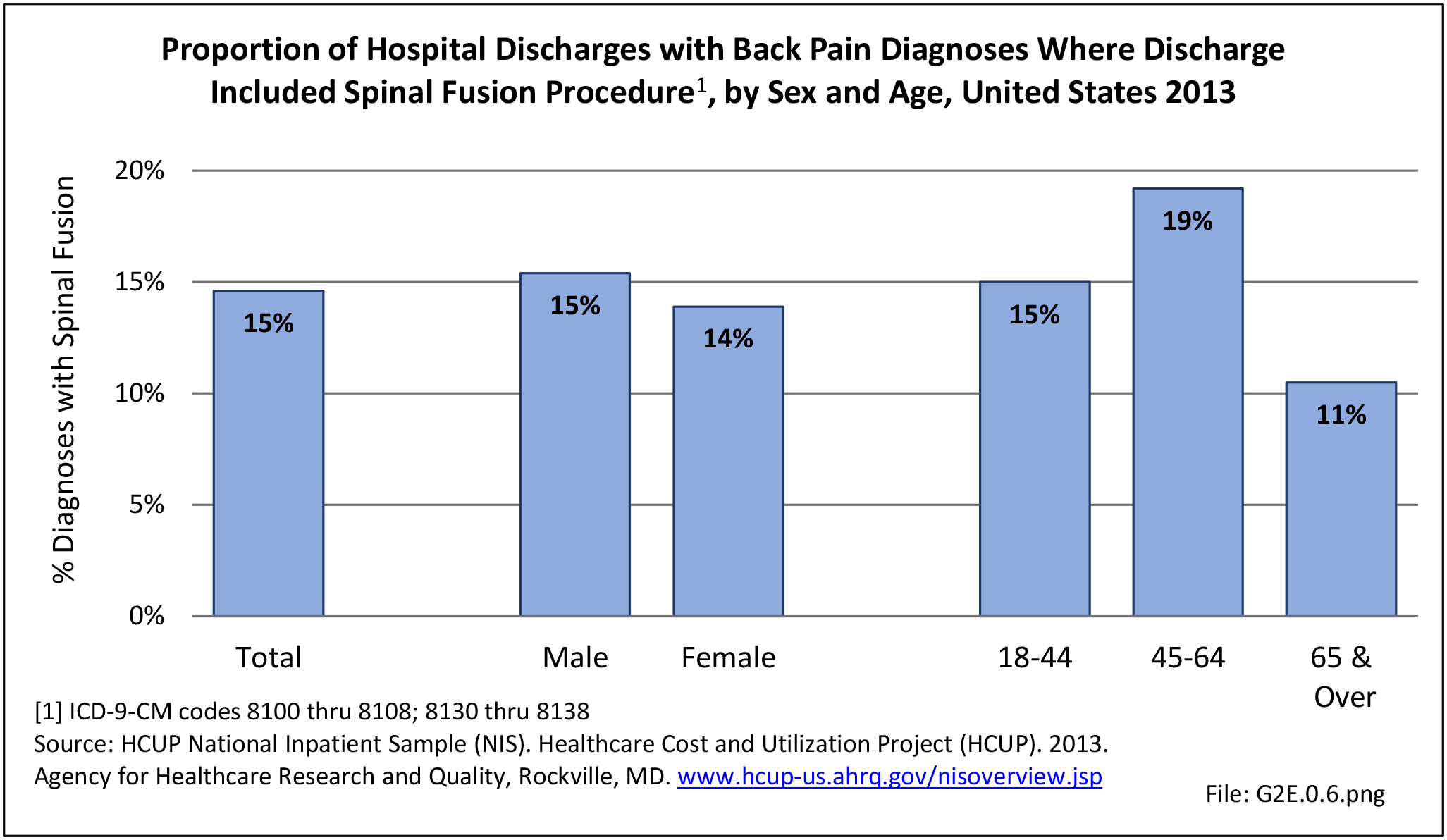
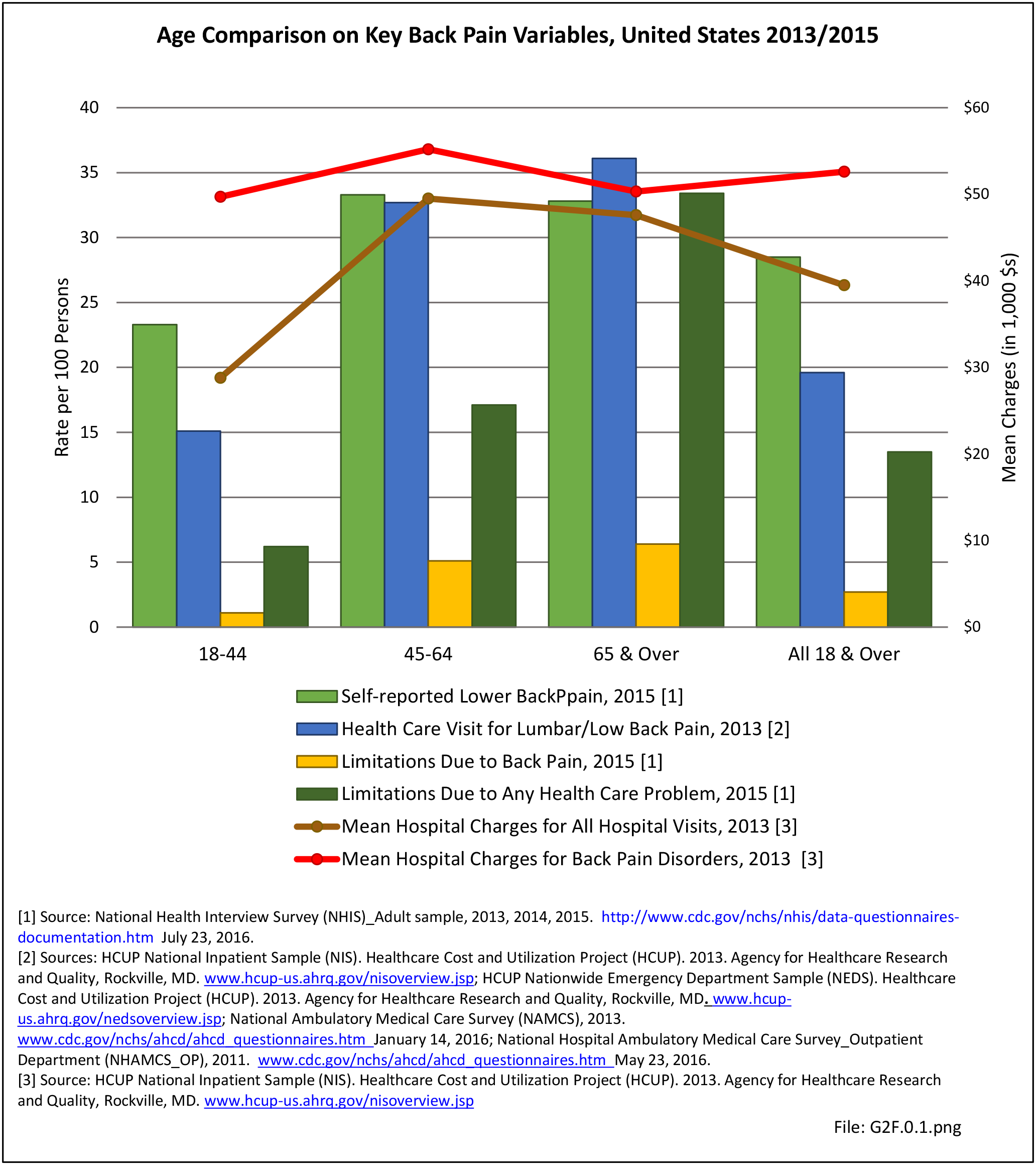
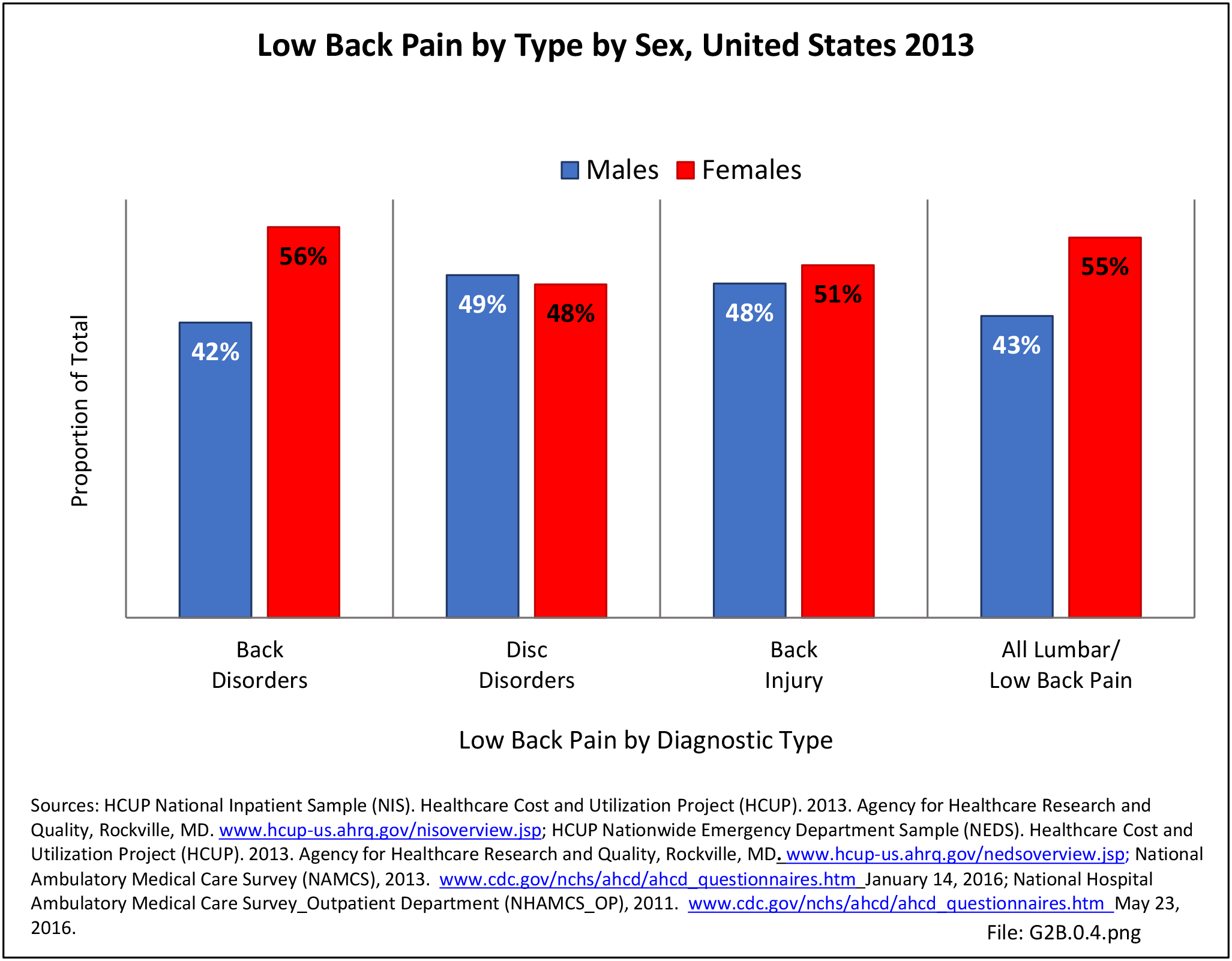
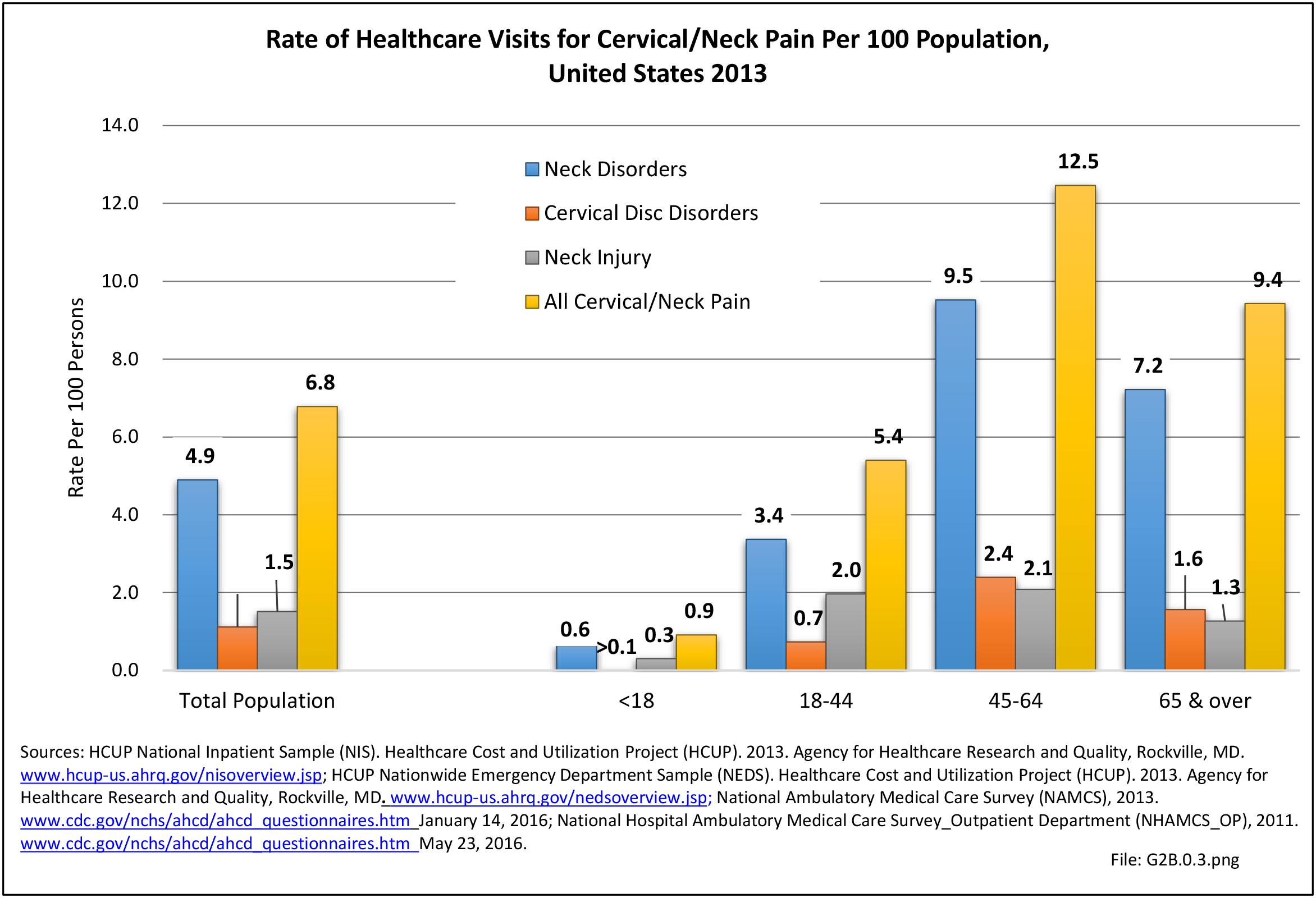
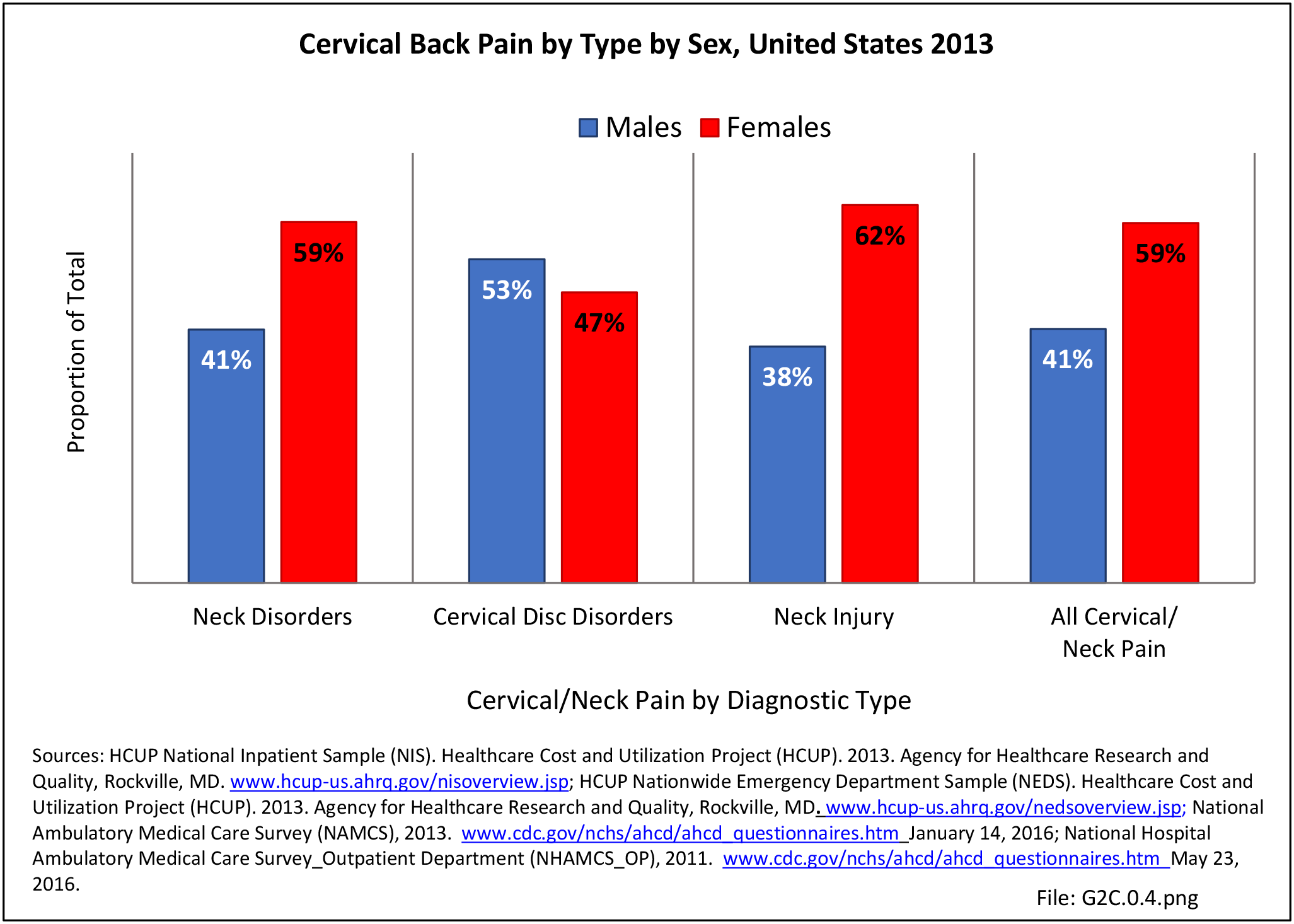
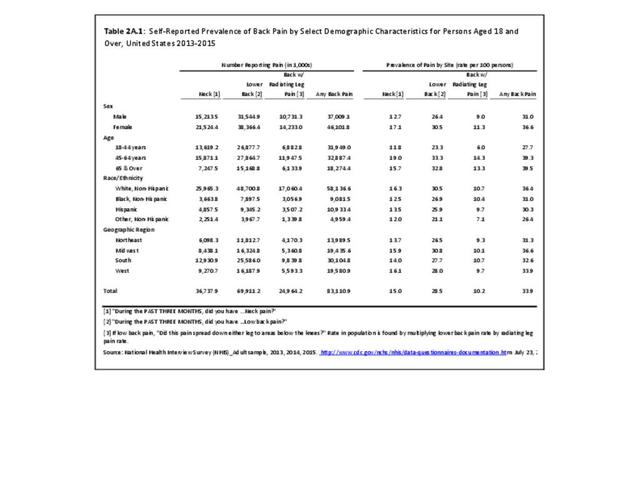
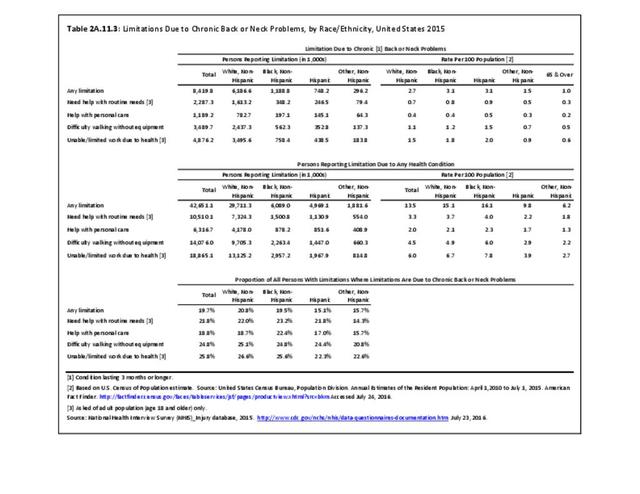
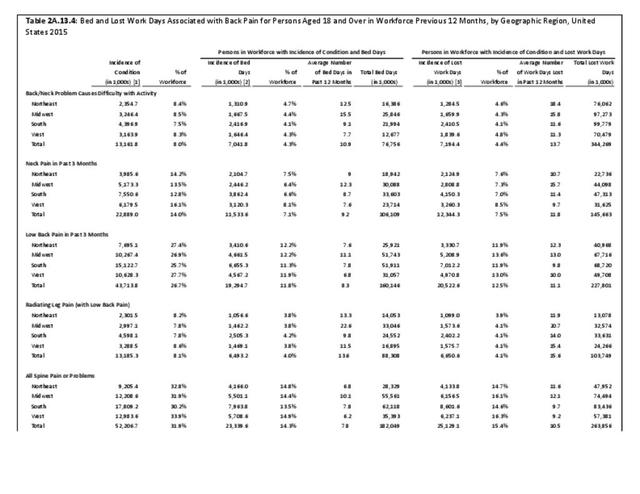
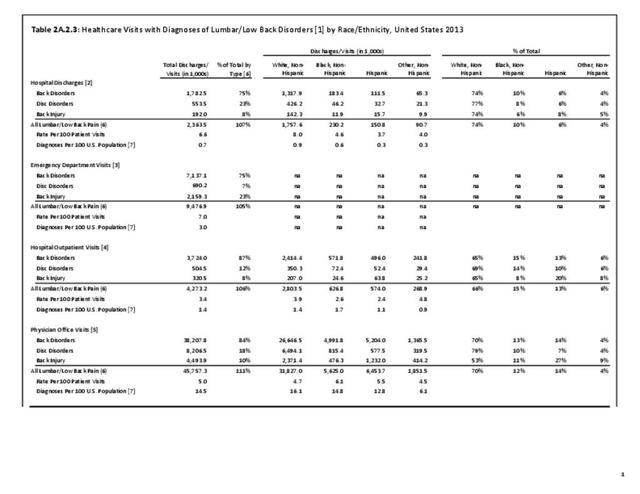
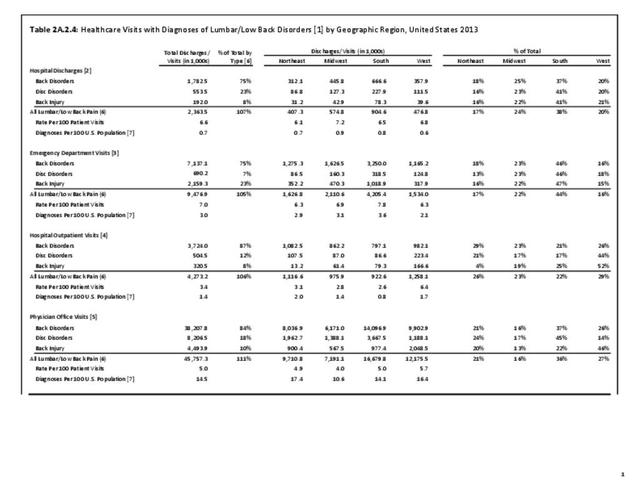
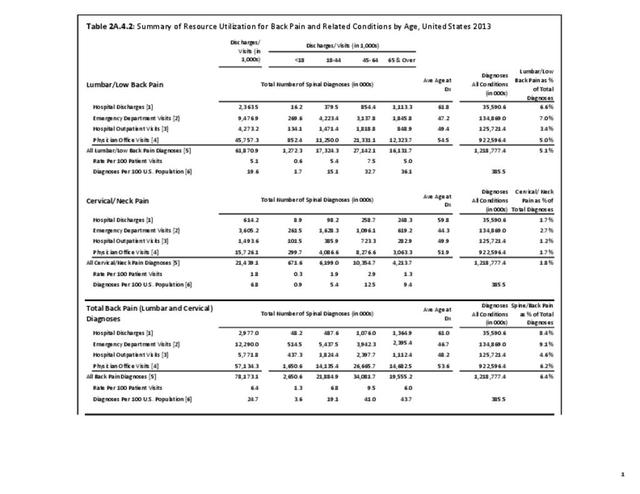
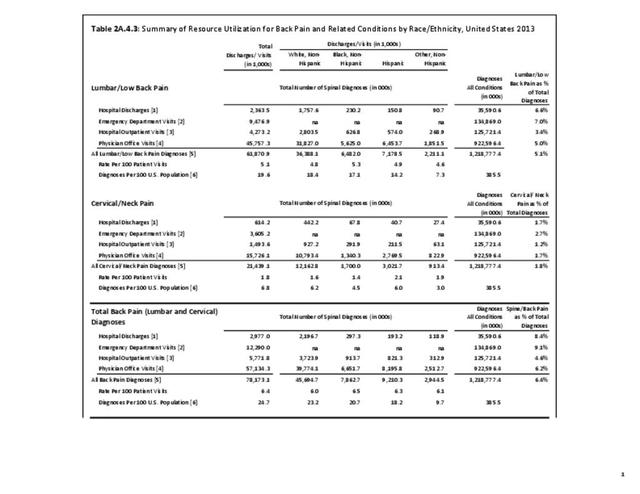
A large healthcare survey is conducted annually in the United States by the National Center for Health Statistics to identify the incidence and prevalence of select health conditions. On average, back pain was reported by 33.9% of persons aged 18 years and older for the years 2013-2015. Low back pain was the most common type of back pain, affecting 28.5%; neck pain was the second most common at 15.0%. The prevalence of back pain has remained stable since 20051 and is measured in response to the question of whether the individual “had low back pain or neck pain during the past three months.” Females report back pain more frequently than males (36.6% vs. 31.0%). The prevalence of low back pain and neck pain is highest for adults aged 65 years and over, but only slightly lower for adults aged 45-64. White, non-Hispanic adults are responsible for the highest prevalence of all back pain at 36.4%. When comparing geographic regions of the US, patients located in the Midwest report back and neck pain at the highest percentage (36.6%). (Reference Table 2A.1 PDF CSV)
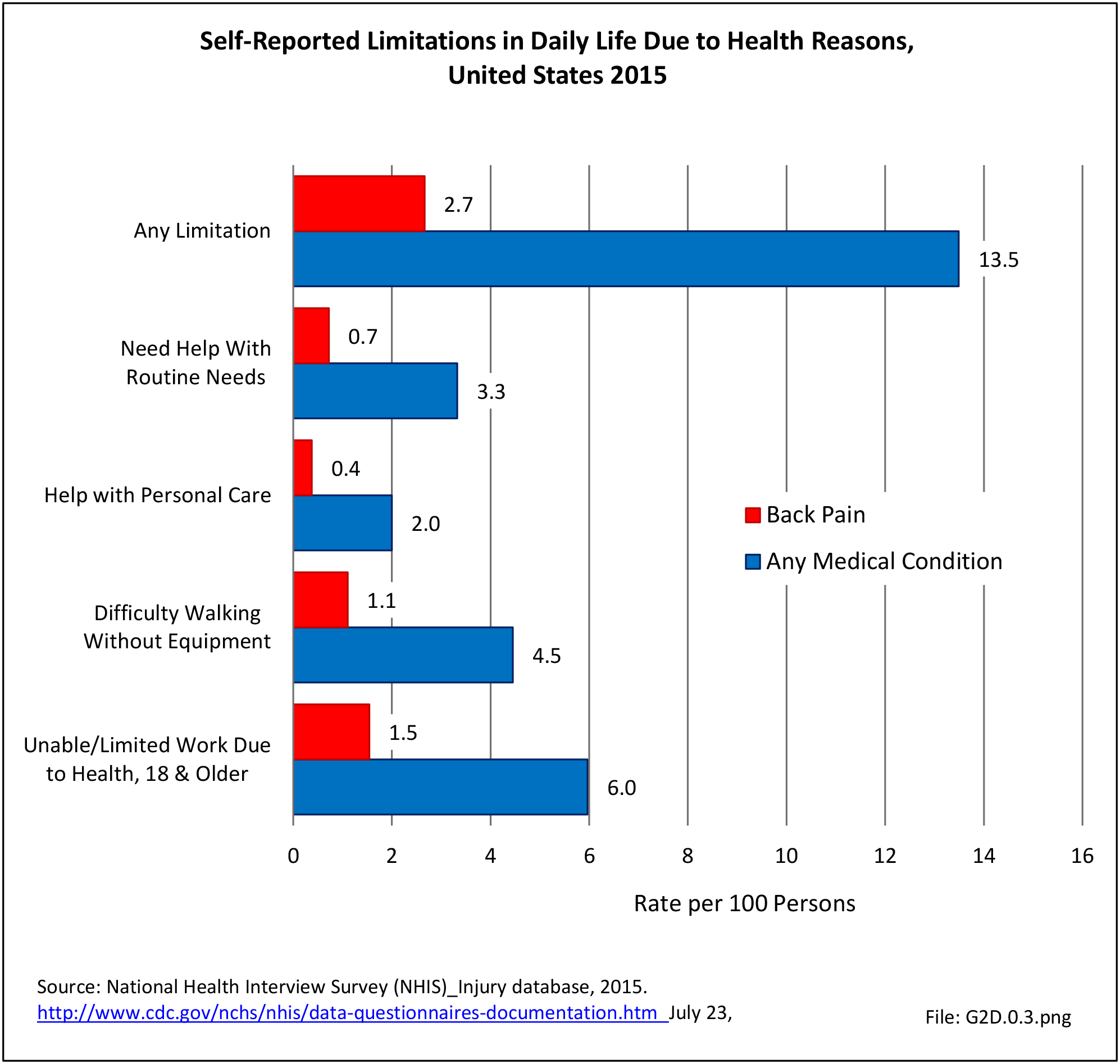
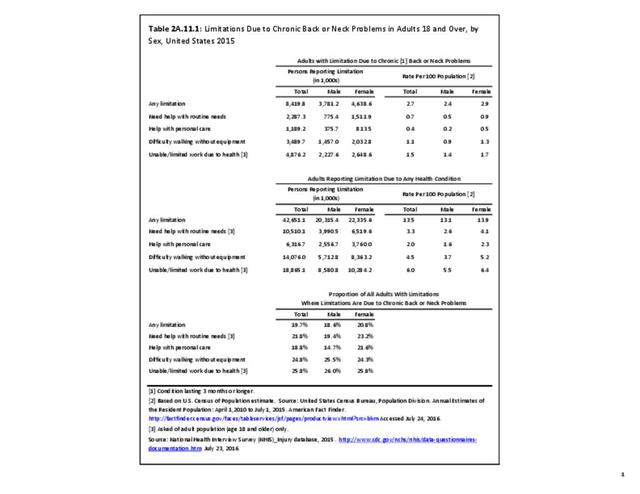
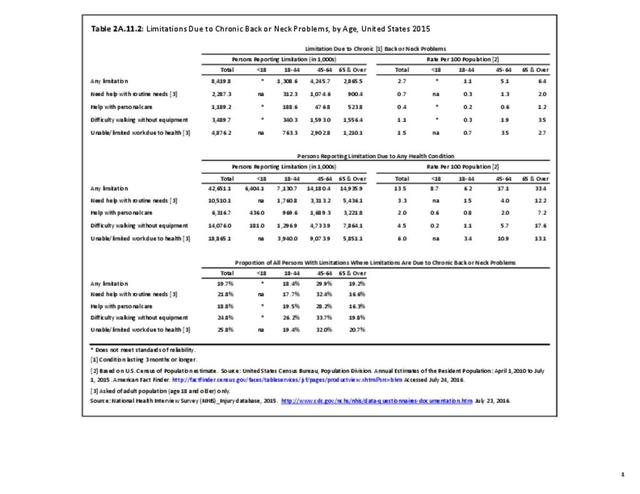
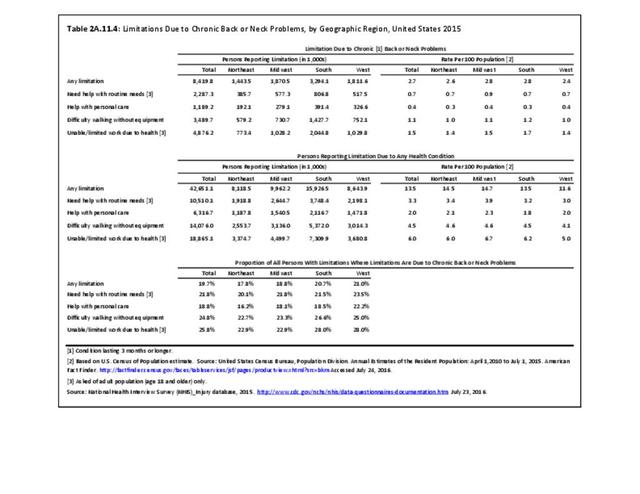
Approximately 1 in 17 persons (6.0%) of the population age 18 or older report they have a health condition that precludes work. Among these adults, 25.8%, or about 4 of the 17, are unable or limited in work due to chronic back or neck problems. (Reference Table 2A.11.1 PDF CSV)
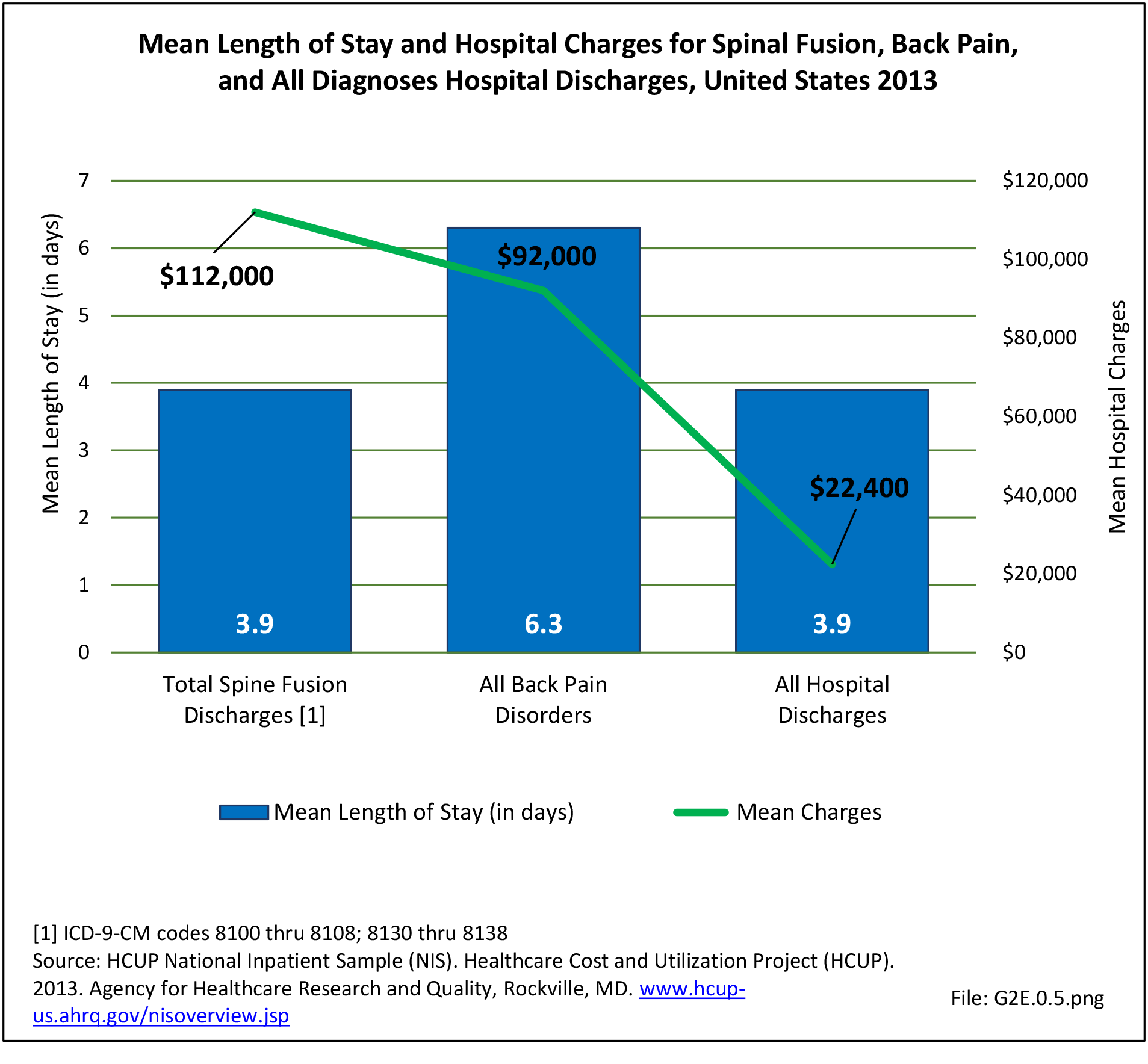
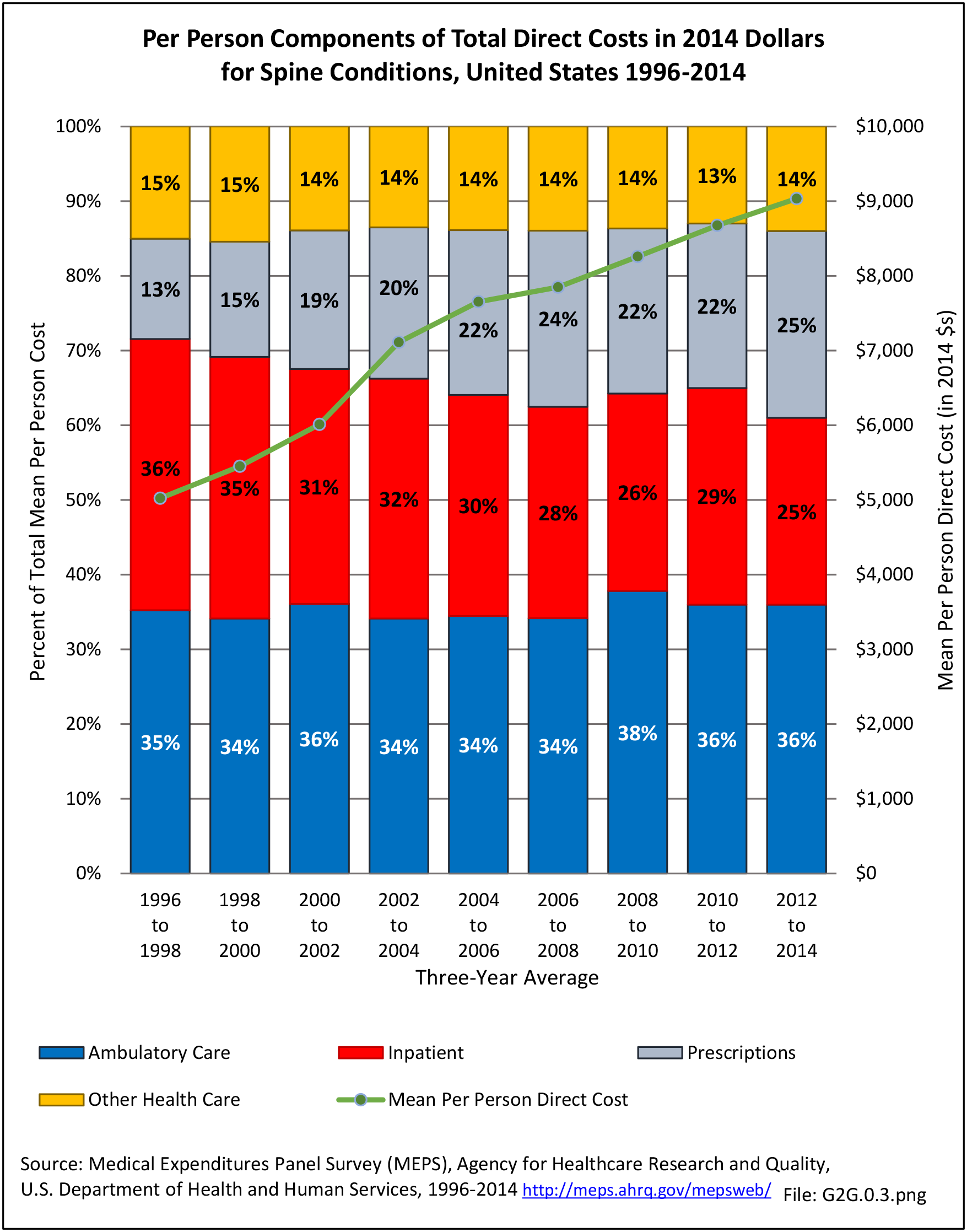
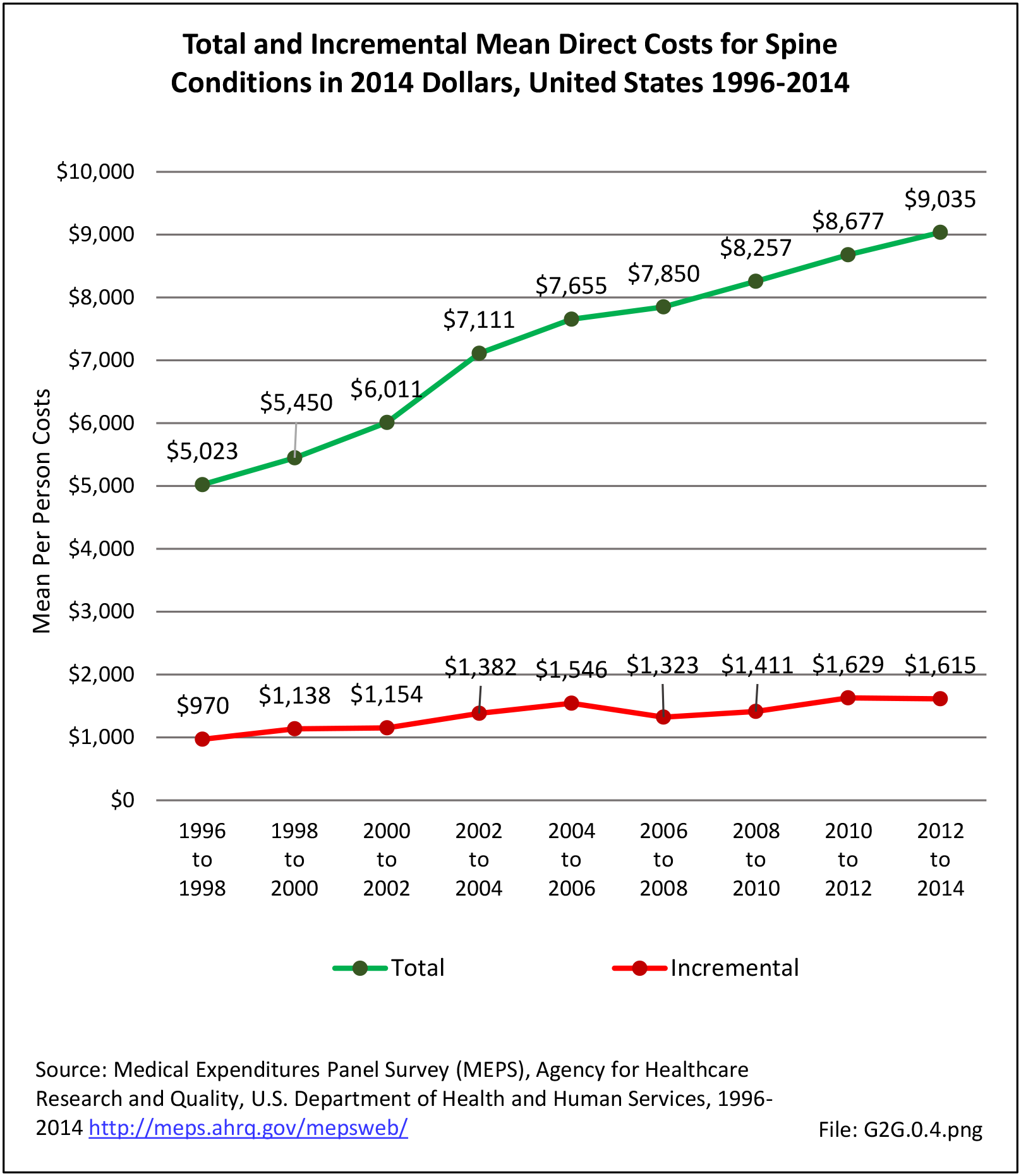
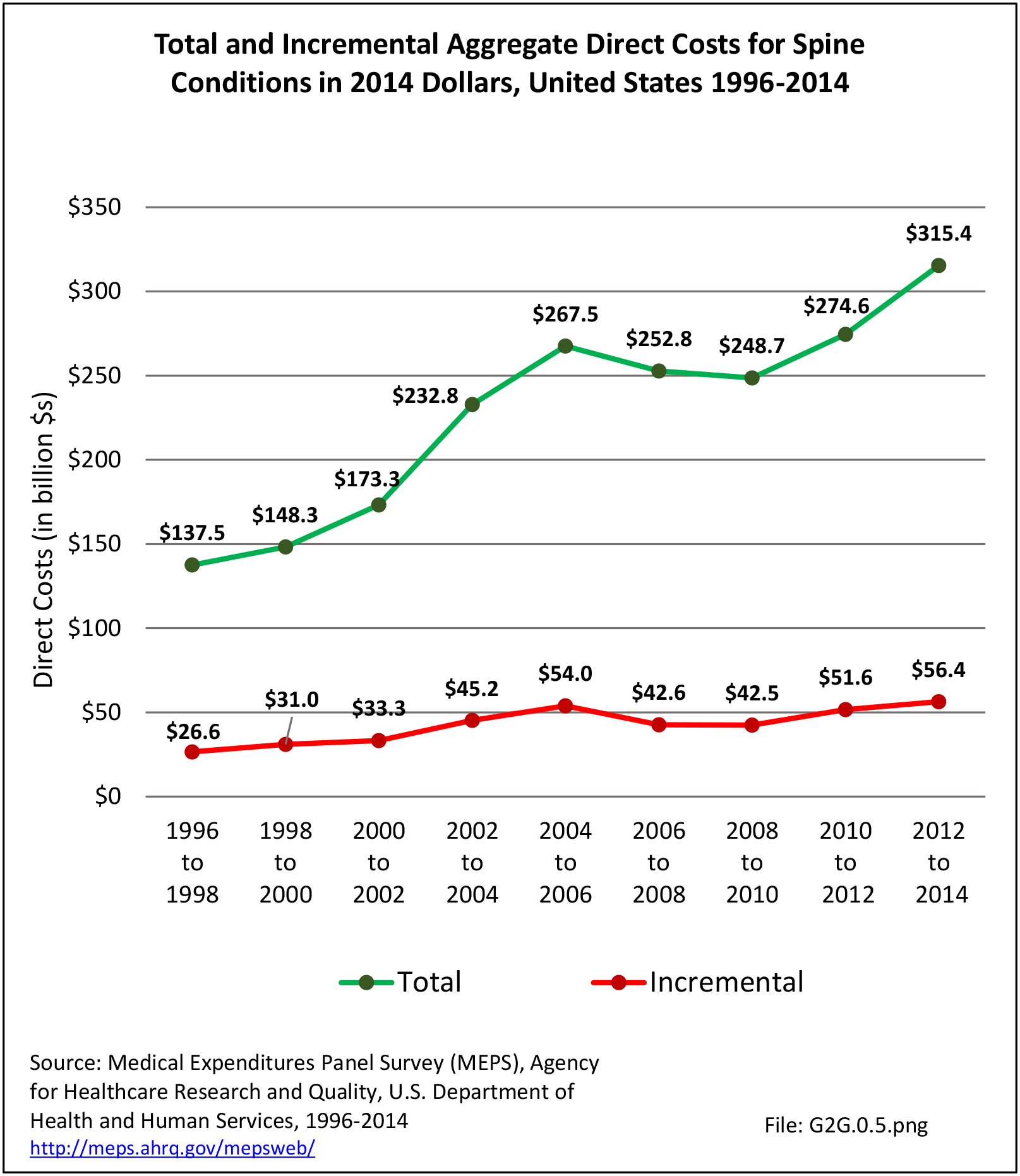
The estimated annual direct medical cost for all persons with a back-related condition in 2014 dollars was an average of $315 billion per year across the years 2012-2014. (Reference Table 8.6.2 PDF CSV) This is further discussed under the Economic Burden topic in this Spine section, and in the Economic Cost topic at this site. As noted previously and elsewhere, this is not the true cost because chiropractic care, physical therapy, alternative therapy, and other care is not included in the analysis. Also, treatment cost from outpatient clinics is currently not available; hence, these data are missing or incomplete.
Back pain often originates from sources that are not readily identifiable. Many causes of back pain are likely related to degenerative changes, but the actual underlying cause of a given back pain episode is often uncertain. In reviewing administrative data for prevalence, it is important to realize that the diagnostic categories may be inaccurate because they reflect differing interpretations about the source of the back pain rather than an absolute diagnosis. This will be discussed further in later sections.
Definitions
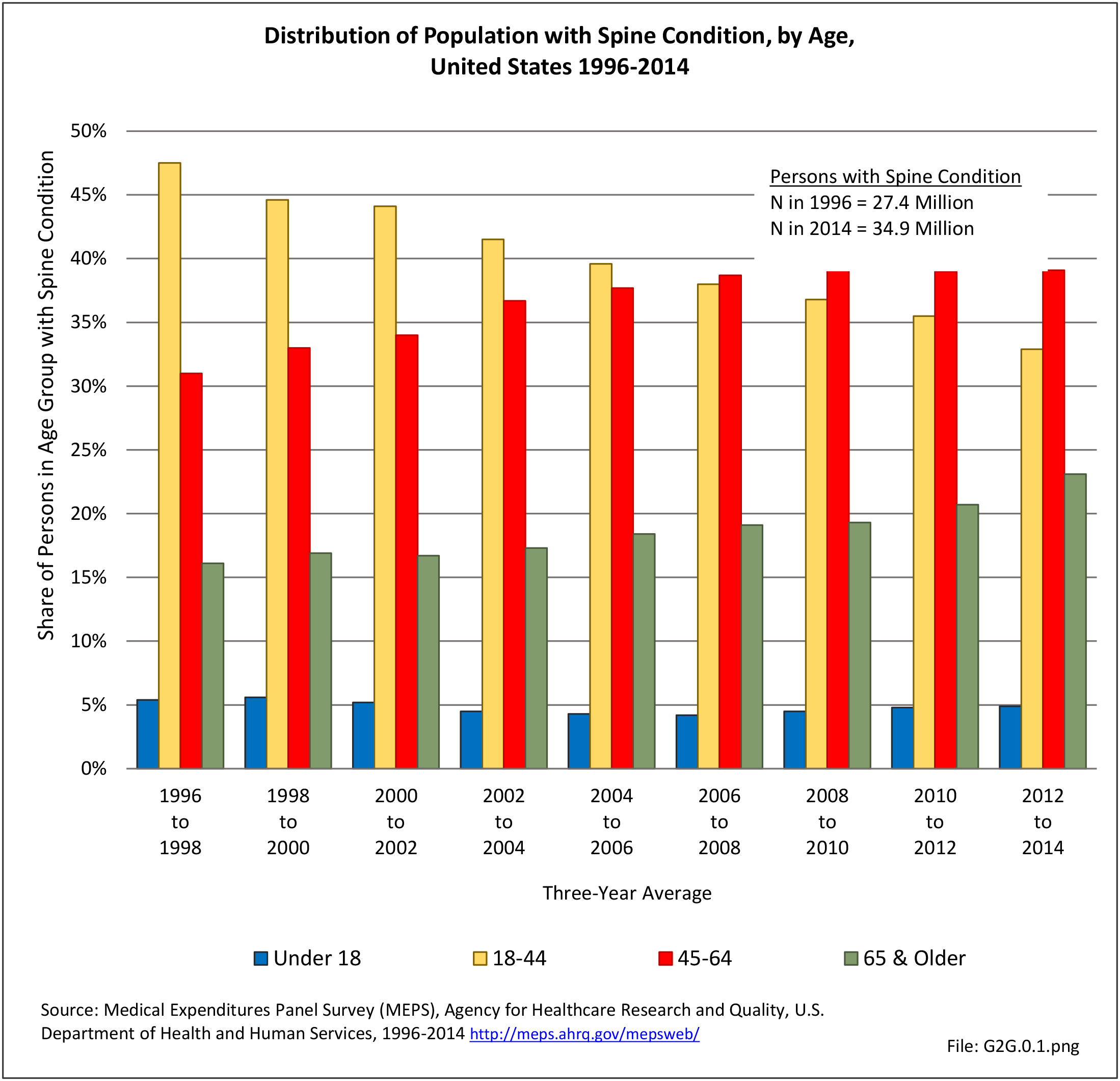
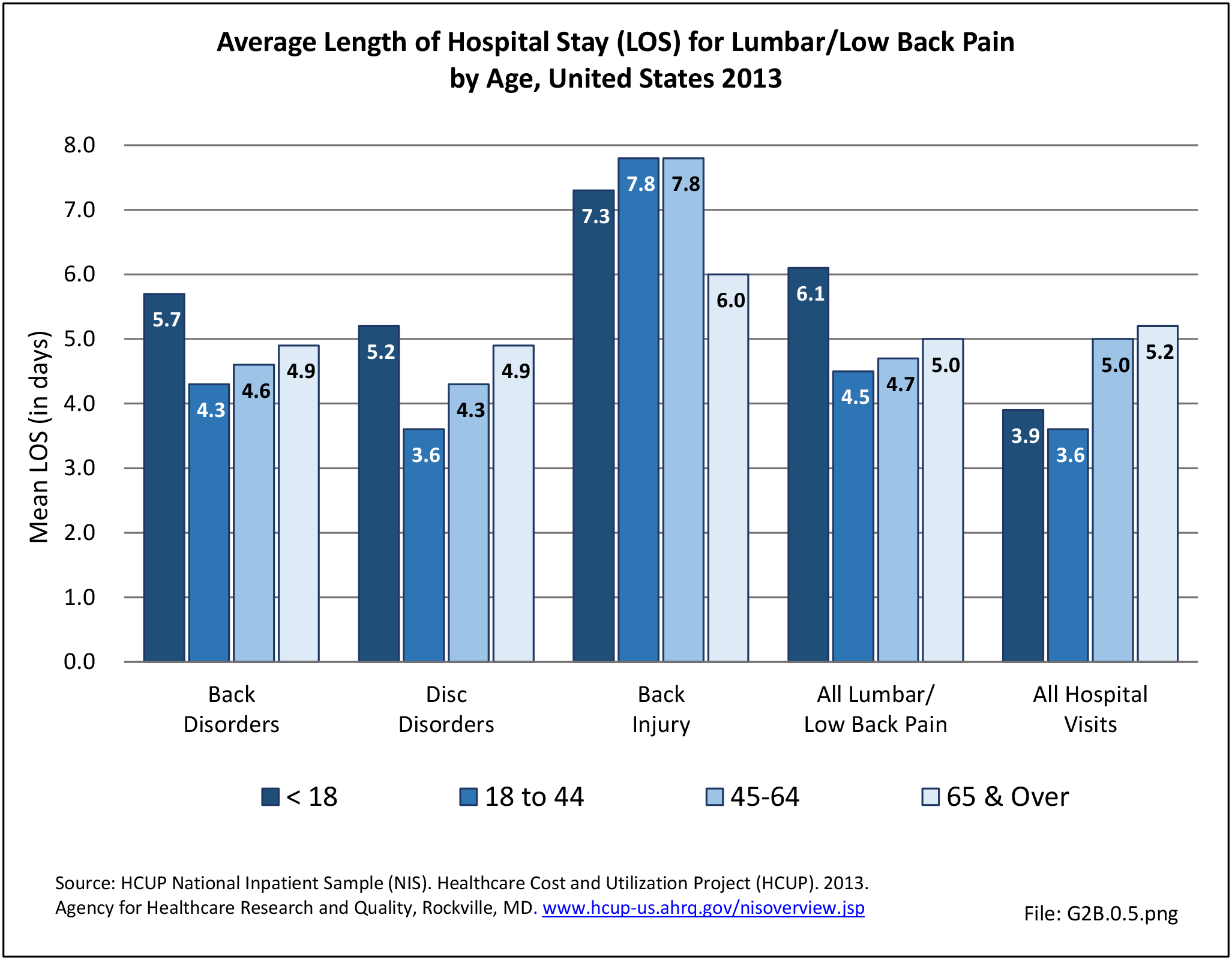
For purposes of further analysis, we decided to divide the diagnostic codes defining the burden of spine problems into three groups: back disorders, disc disorders, and back injuries. This approach allows comparison to earlier editions of the text. We are aware there may be substantial overlap, and that some of the back disorders may be related to degenerative disc changes and some of the disc disorders may have another origin. The role of disc degeneration in the cause of back pain remains uncertain. Intervertebral disc degeneration and associated facet joint osteoarthritis seem to be a natural process of aging but can alter the biomechanics and function of the spine. Studies have identified a strong genetic predisposition, but there are modifying influences including age, obesity, smoking, and genetics.
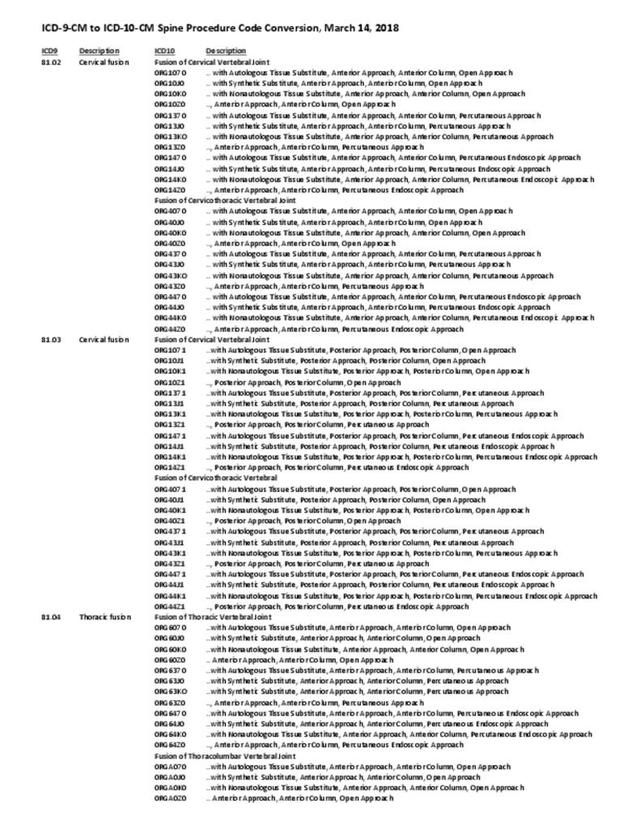
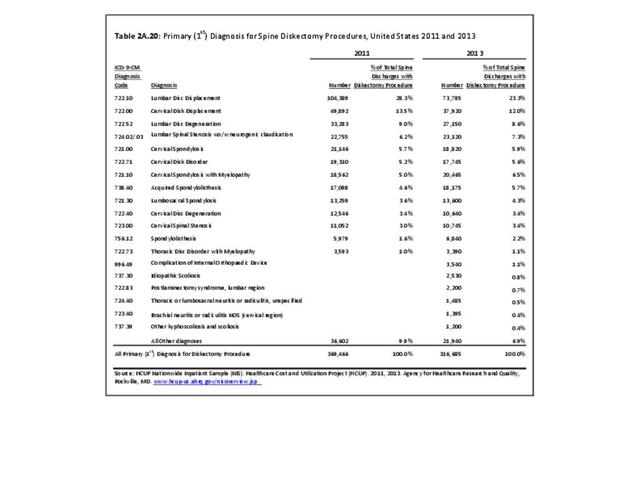
In the tables and text, we define back disorders by diagnostic ICD-9-CM Codes 720, 721, and 724. These codes include inflammatory spine conditions, spondylosis, spinal stenosis, lumbago, sciatica, backache, and disorders of the sacrum. Disc disorders include herniations, disc degeneration, and post-laminectomy syndromes (ICD-9-CM Code 722). Back injuries include fractures, dislocations, and sprains (ICD-9-CM Codes 805, 806, 839, 846, and 847). The same classifications are used for both low back pain and neck pain. Thoracic back pain, or upper and middle back pain associated with the 12 spinal bones connected to and in the same level in the body as the 12 ribs, is less common and not as well studied. Data associated with thoracic spine pain is generally included in the analysis of low back back and disc disorders and injuries.
Unfortunately, the databases do not permit diagnostic verification. Sometimes diagnoses are provided primarily for reimbursement purposes, with little emphasis on accuracy. Further, there is considerable overlap. For example, a patient with back pain of unknown origin could be given the diagnosis of lumbago, placing him or her in the back disorder category. He or she may also have disc degeneration with a diagnosis of degenerative disc disease and, therefore, be placed in the disc disorder category. Or, if his or her problem developed after a lift or twist, it could be diagnosed as a back strain, falling into the back injury category.
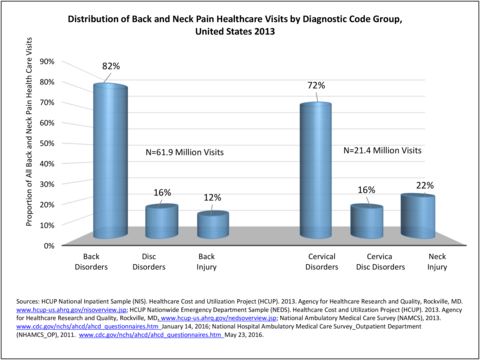
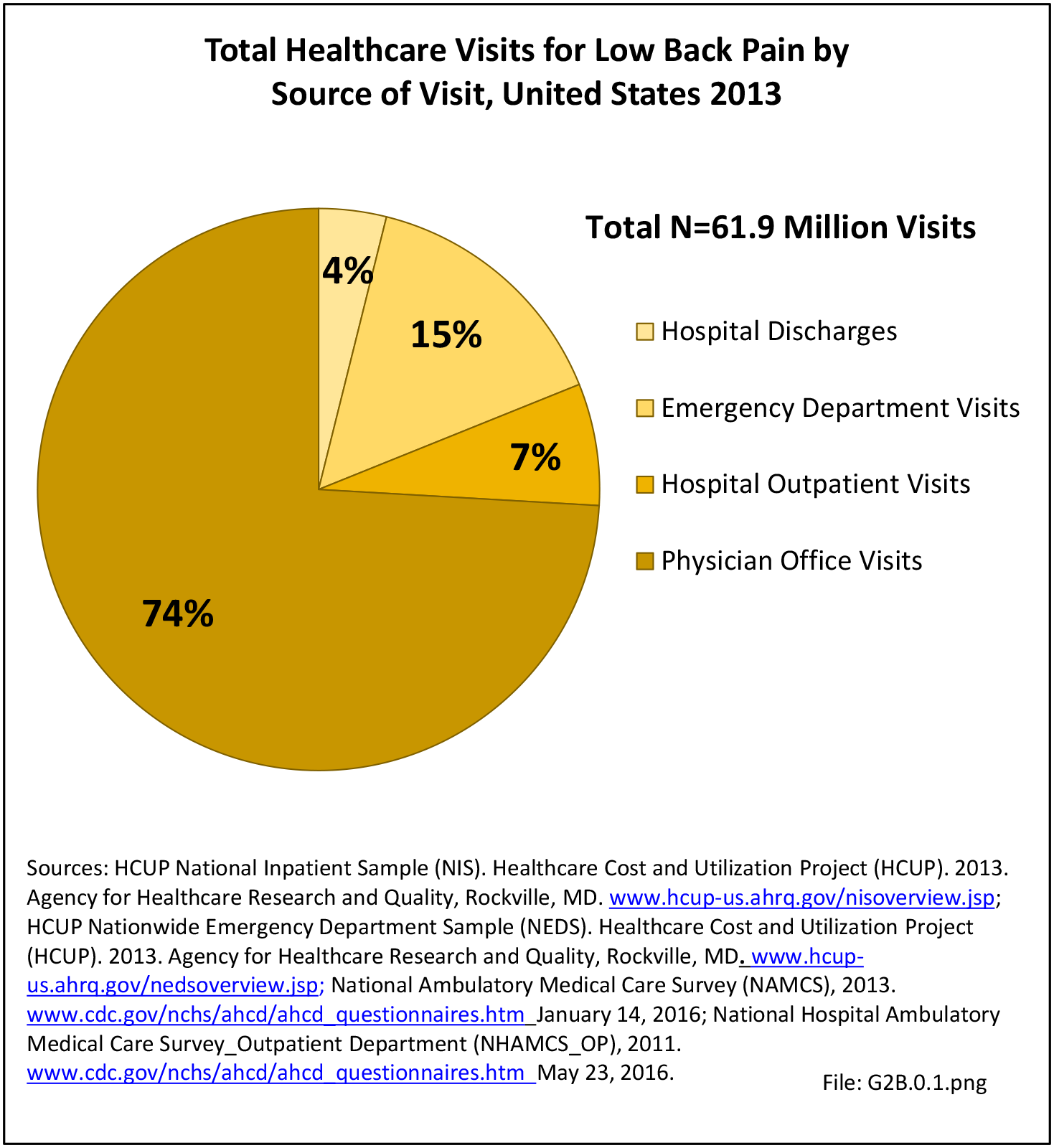
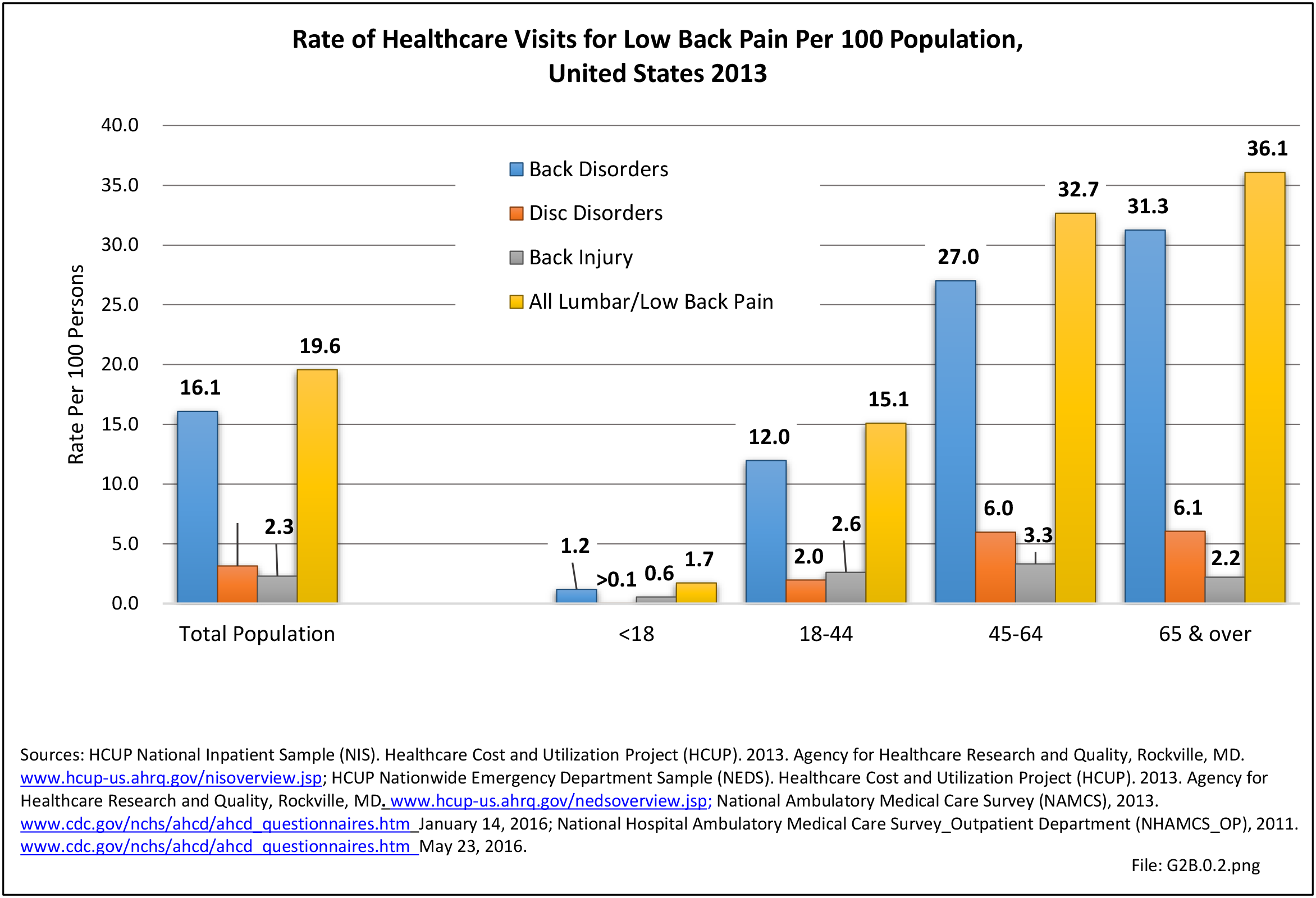
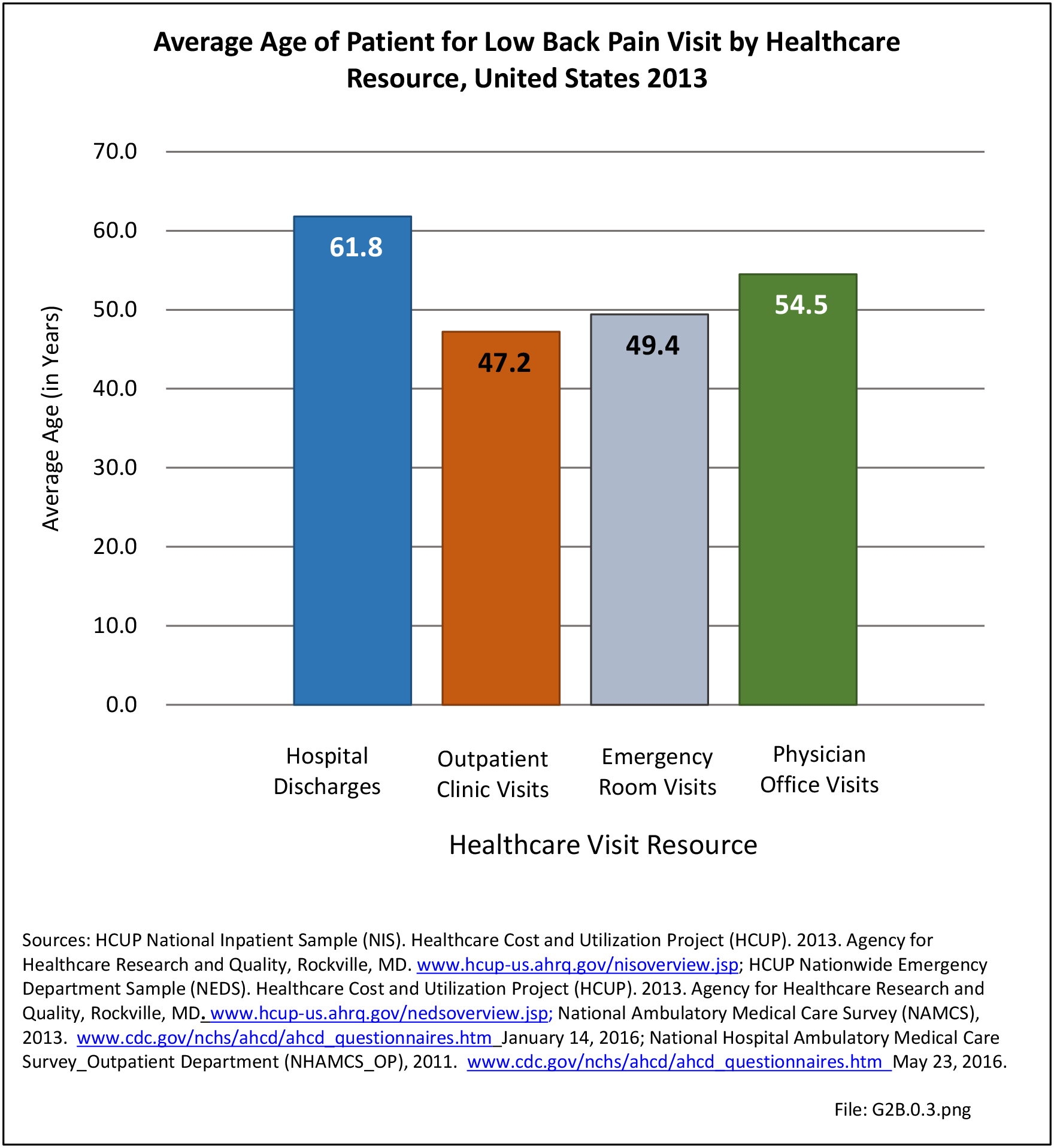
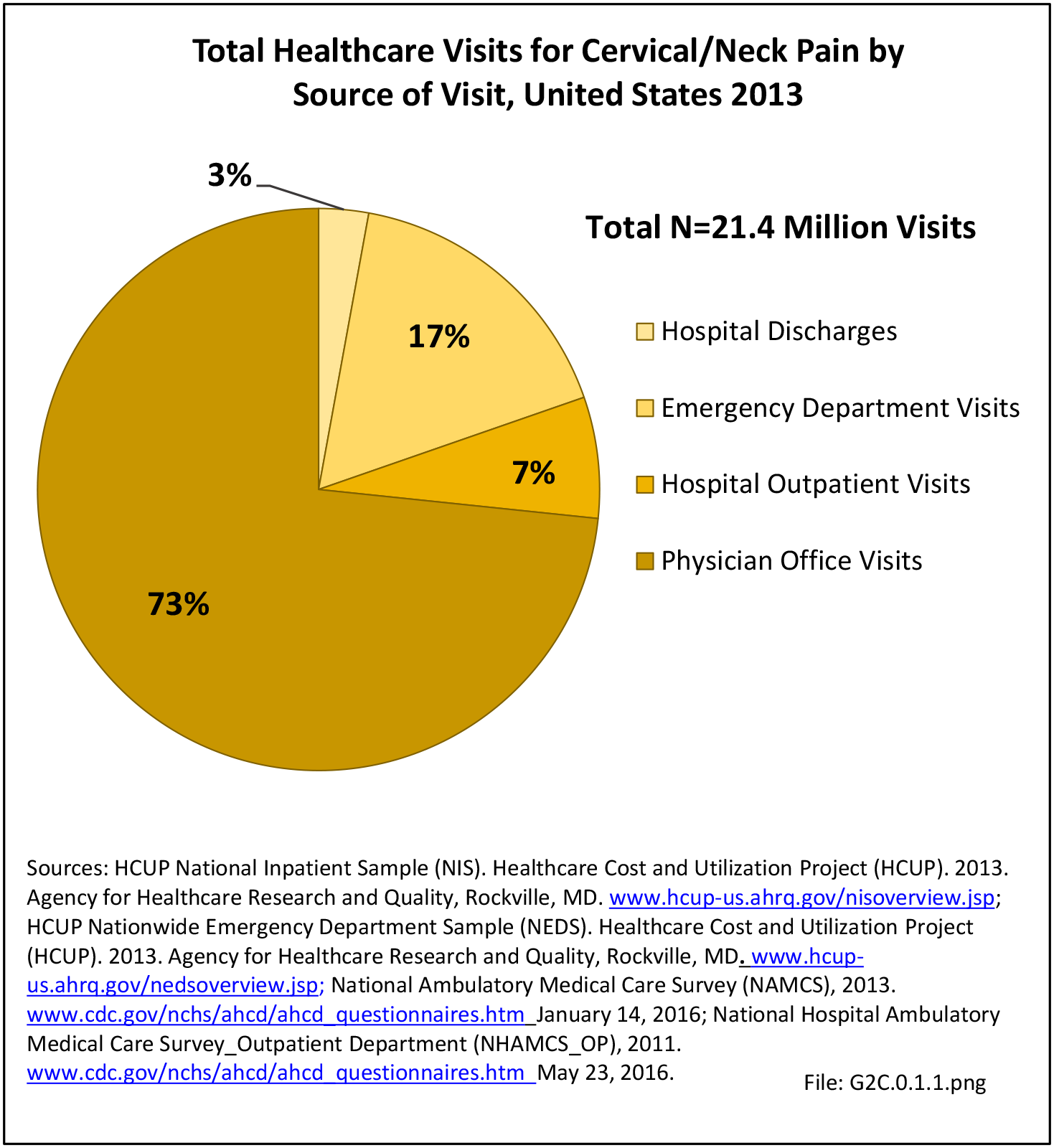
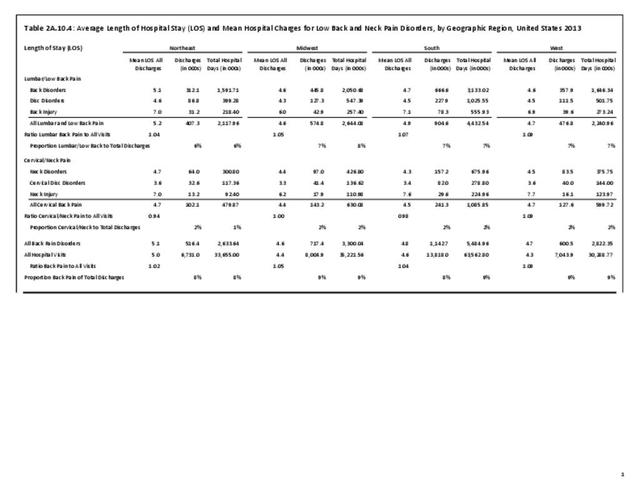
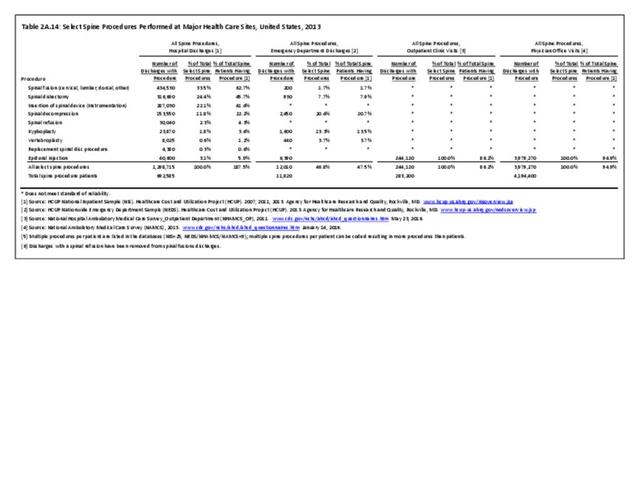
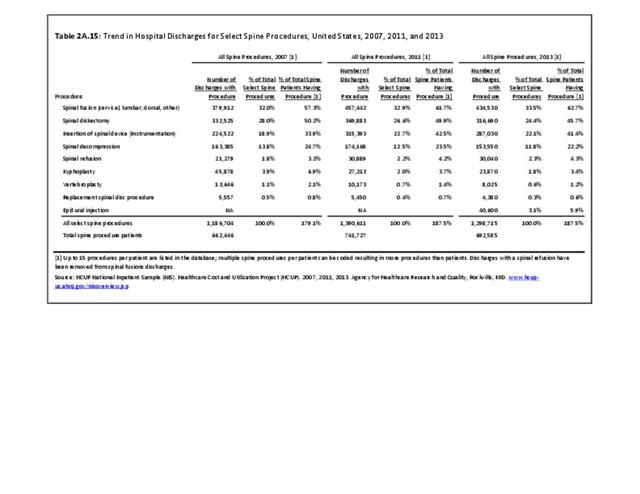
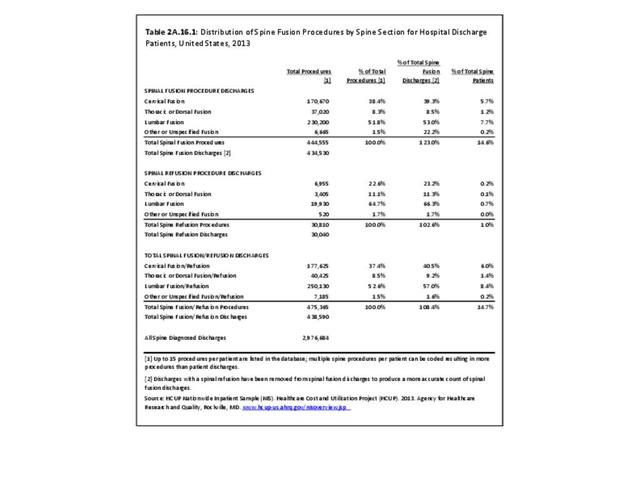
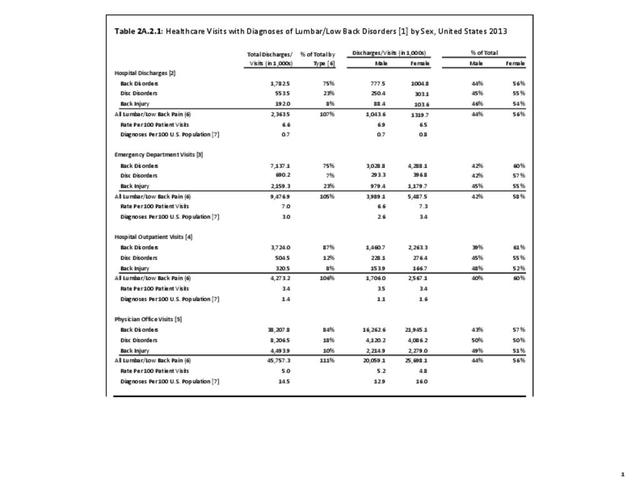
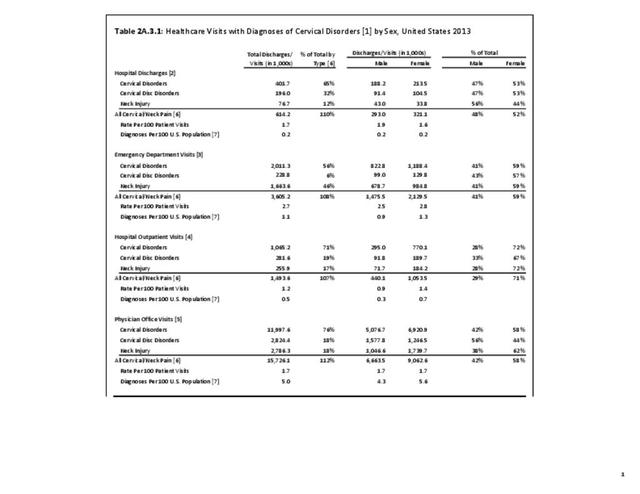
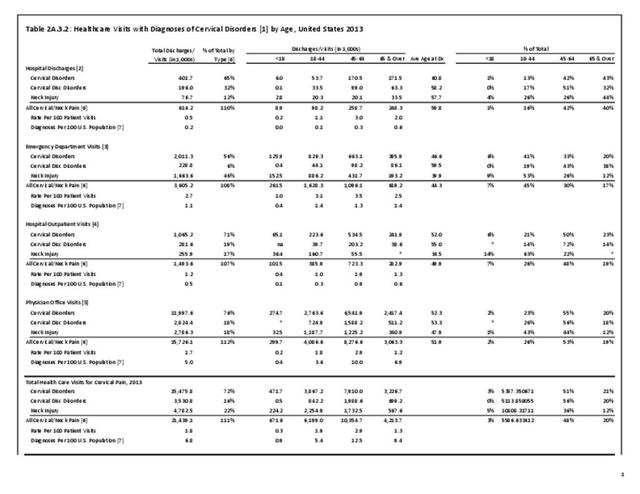
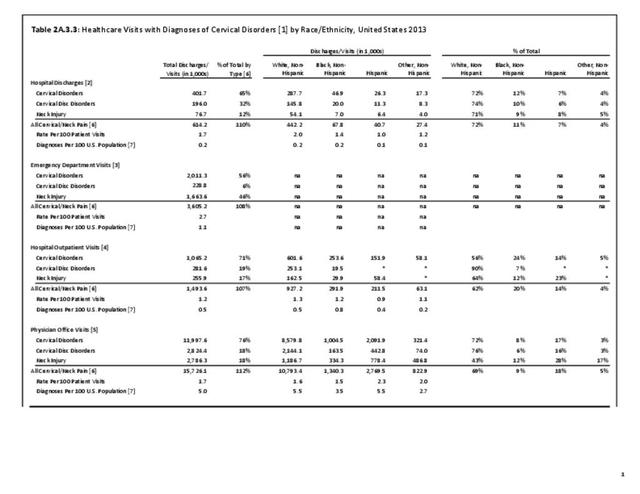
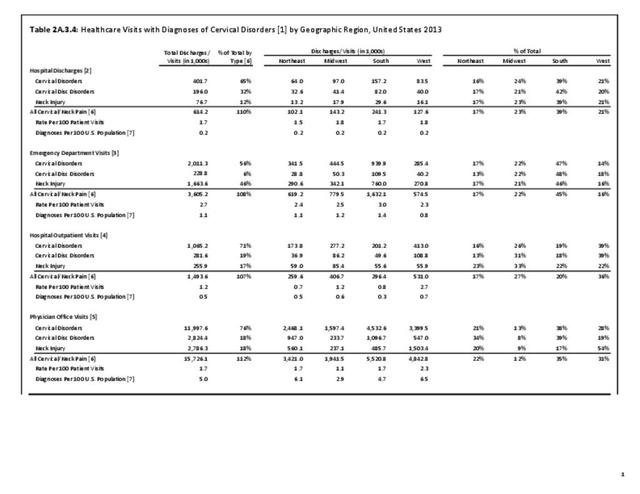
In the tables and graphs, total healthcare visits include hospital discharges obtained from the 2013 Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample, emergency department visits obtained from the 2013 HCUP Nationwide Emergency Inpatient Sample, hospital outpatient visits obtained from the 2011 National Hospital Ambulatory Medical Care Survey Outpatients (NHAMCS-OP), and physician office visits obtained from the 2013 National Ambulatory Medical Care Survey (NAMCS).
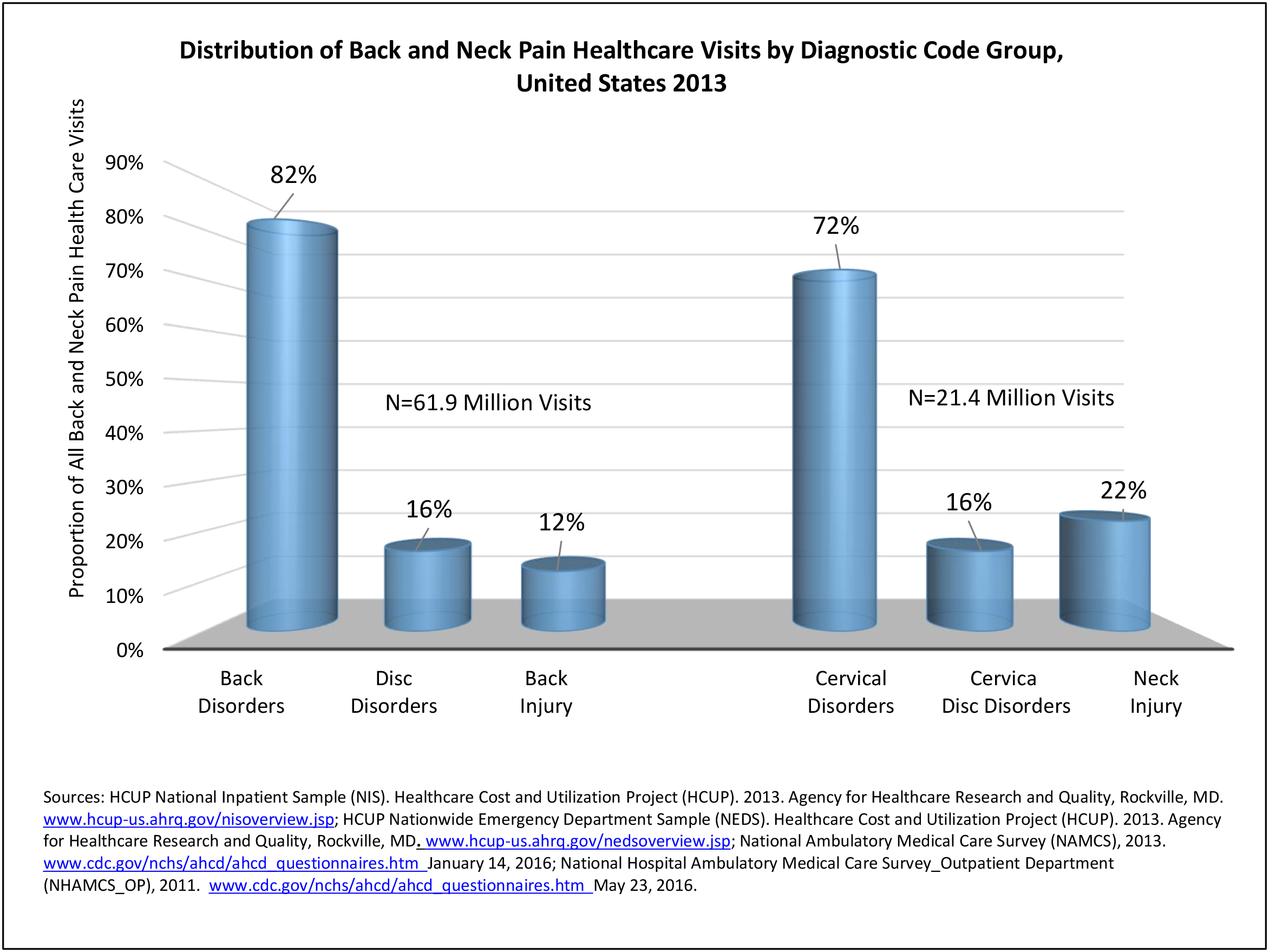
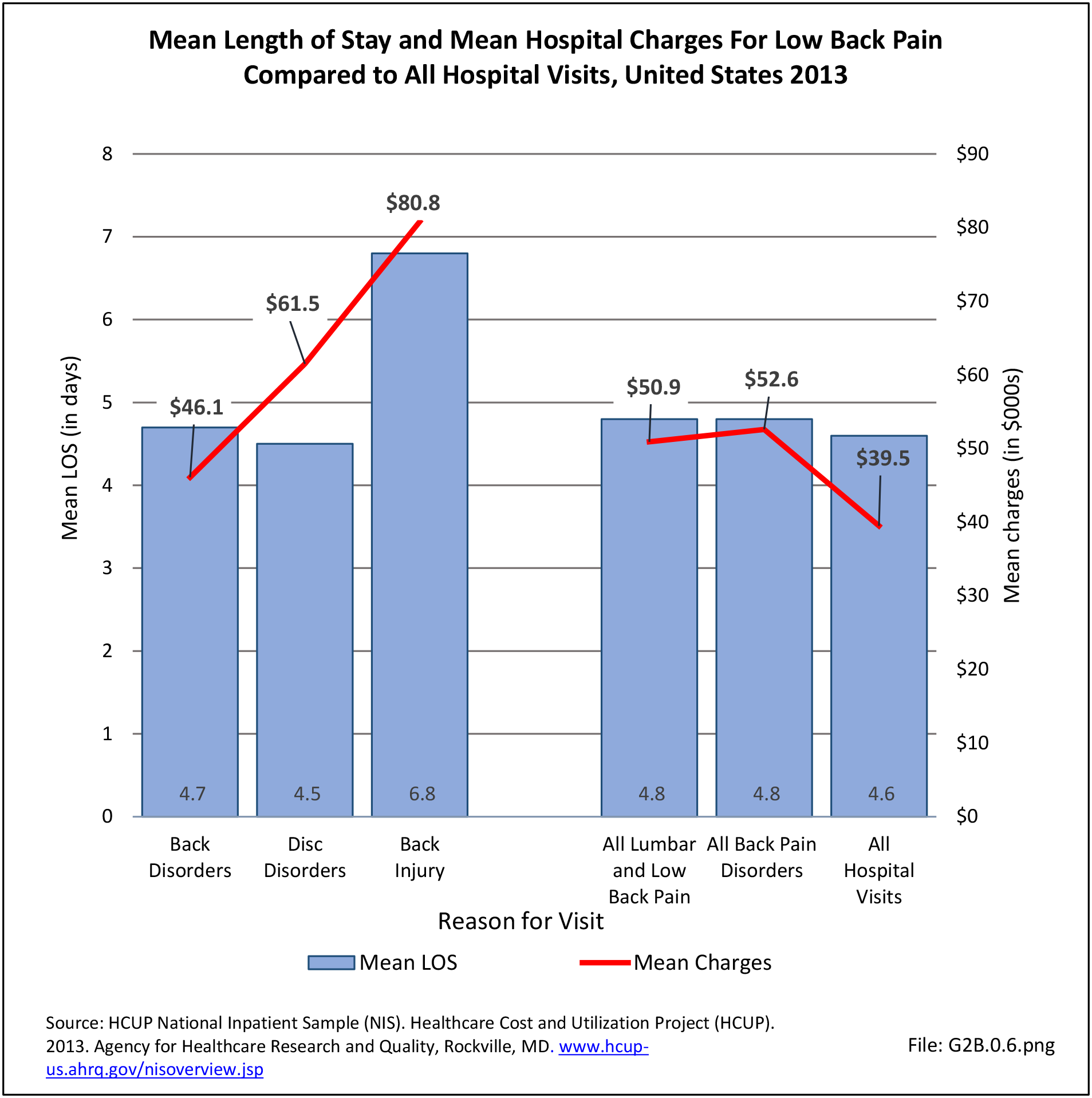
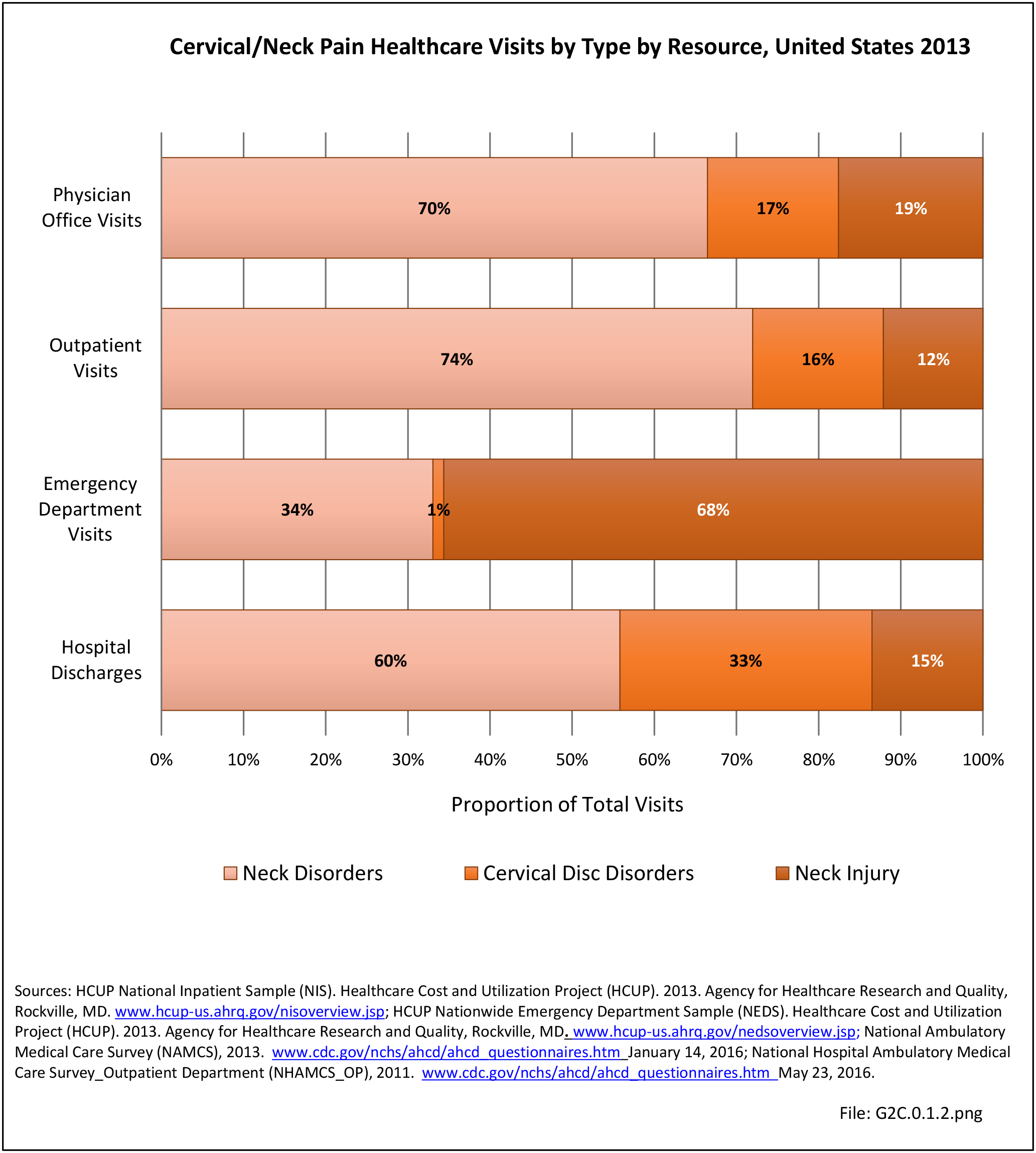
Using the diagnostic code grouping discussed above, back disorders accounted for 82% of low back pain healthcare resource utilization in 2013. Back disorders accounted for 75% of hospitalizations. Disc disorders accounted for 16% of low back pain resource visits, and approximately 23% of hospitalizations. Emergency department visits for disc disorders were not common, comprising only 7% of all back pain-related visits. Back injuries, which include fractures, sprains, and strains, are often reported as caused by overexertion or overuse. They accounted for the remaining 12% of 2013 low back pain resource visits. Back injuries were most commonly seen in the emergency room (23%), but constituted only 8% of hospitalizations, indicating that most were manageable in an outpatient setting, and were most likely soft tissue injuries. (Reference Table 2A.2.1 PDF CSV)
- 1. United States Bone and Joint Decade: The Burden of Musculoskeletal Diseases in the United States, First Edition. Rosemont, IL, American Academy of Orthopaedic Surgeons, 2008, p. 42.
Edition:
- Fourth Edition