Neuromuscular disorder (NMD) is a collective term used to describe diseases that affect any part of the nervous system and muscles. Although there are many different forms that vary in onset, severity, and prognosis, NMDs can have a significant direct and indirect impact on an individual leading to loss of functional capacity.1
Definitions
Different classification systems are available for neuromuscular disorders based on the location of involvement, the etiology, or presenting symptom. Based on the anatomic location of involvement, NMD can be categorized into
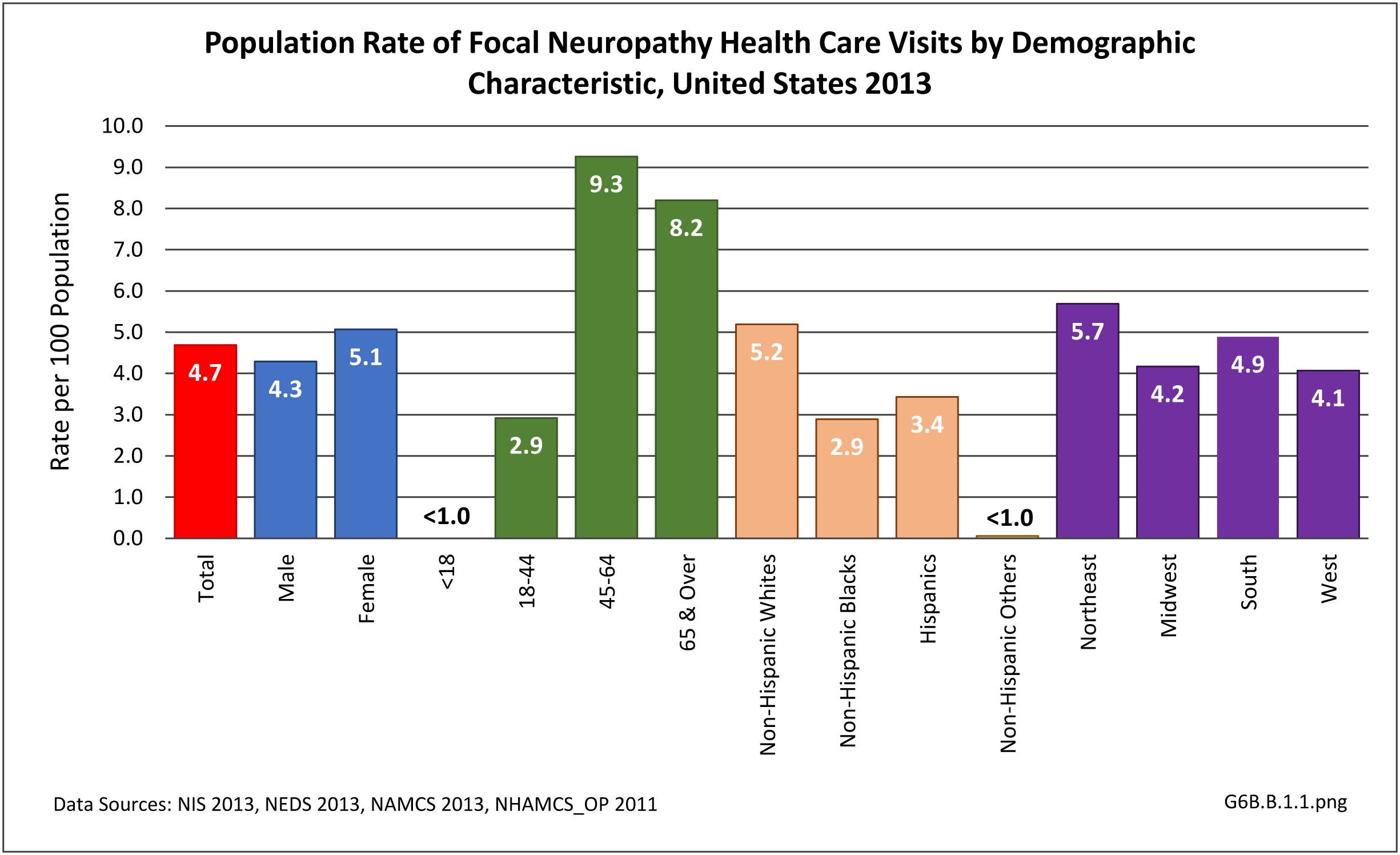
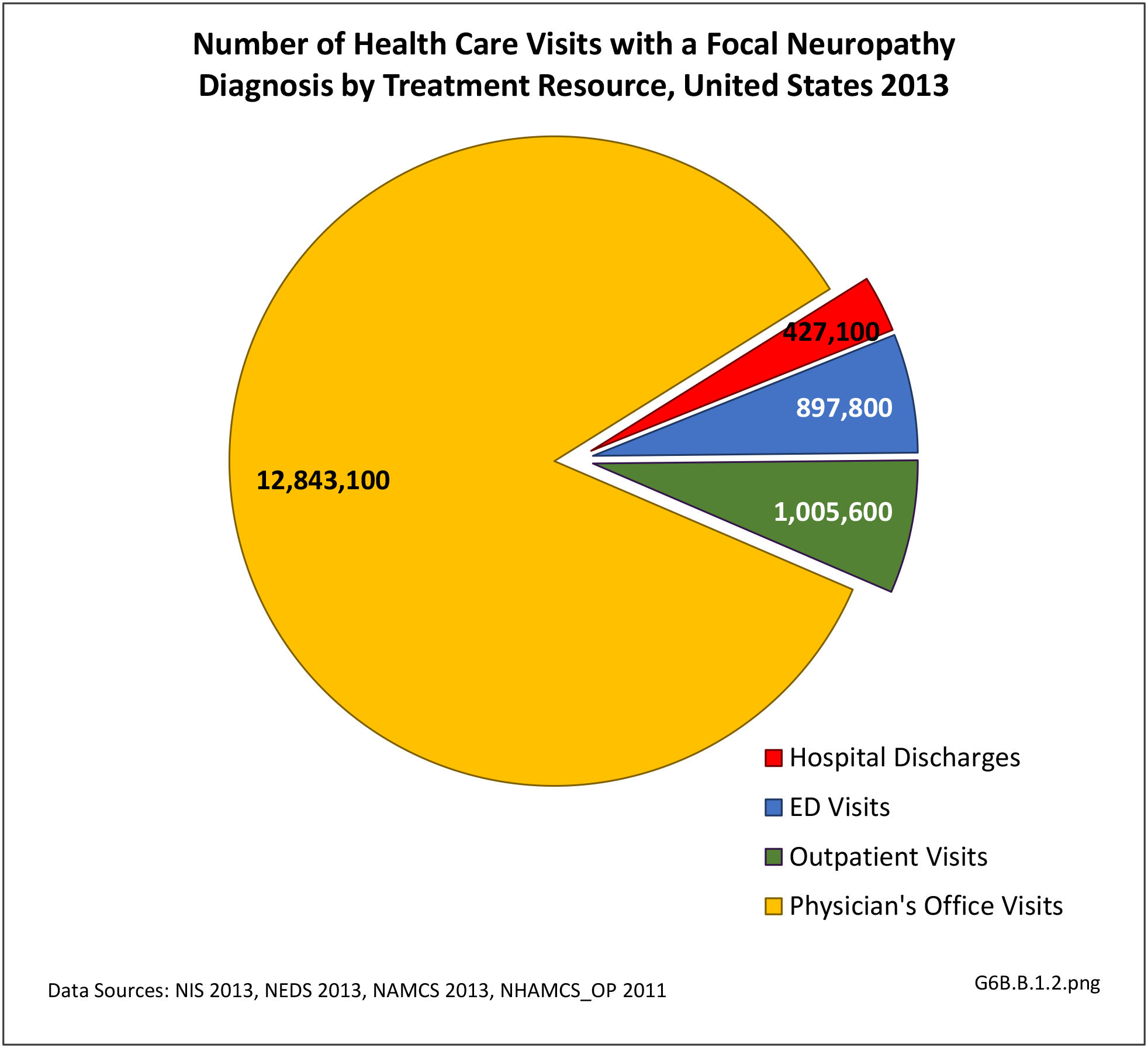
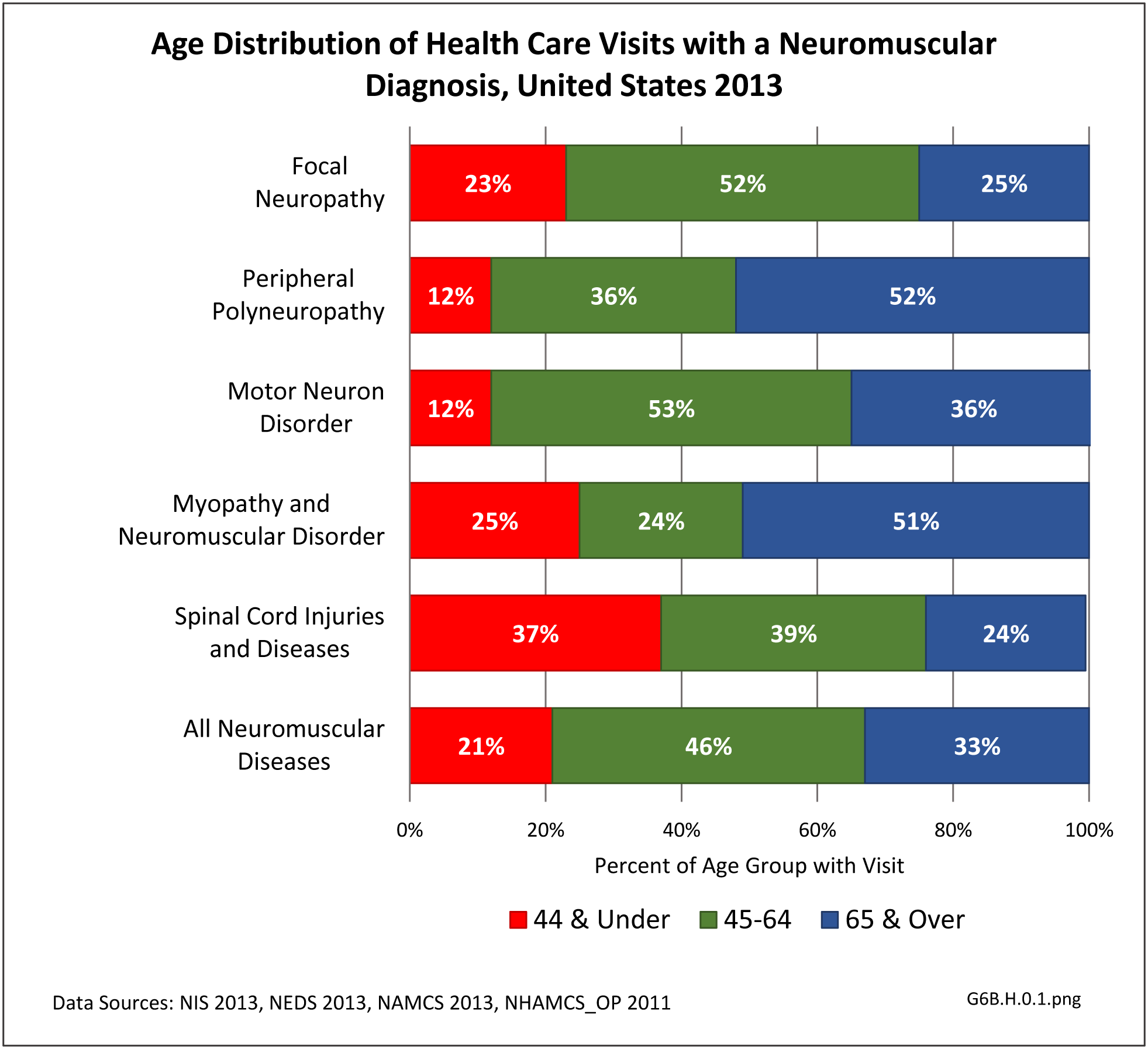
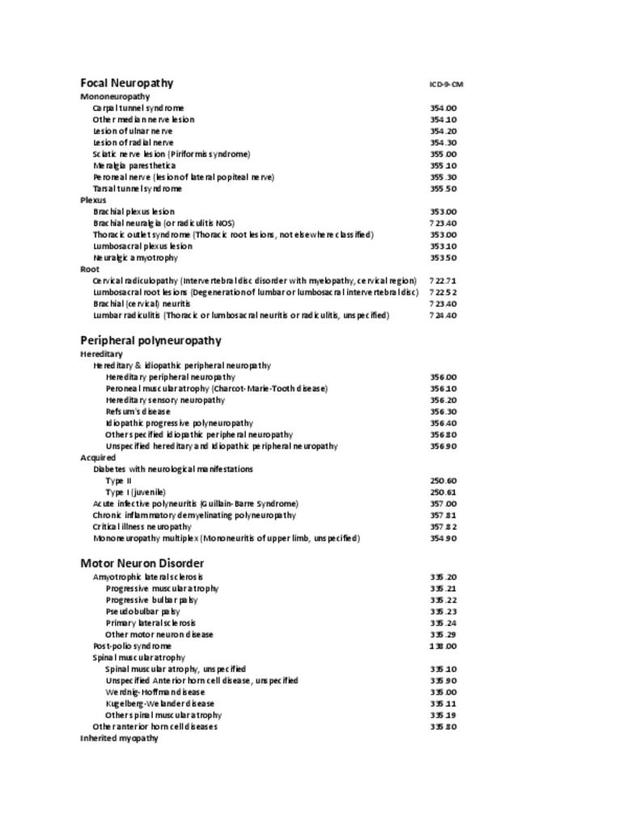
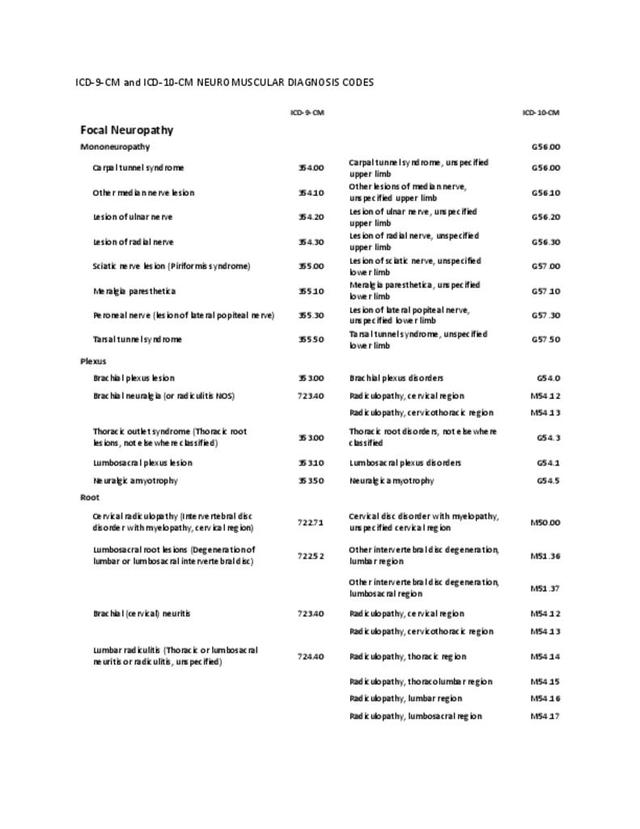
- focal neuropathy, involving one site or confined to a single limb;
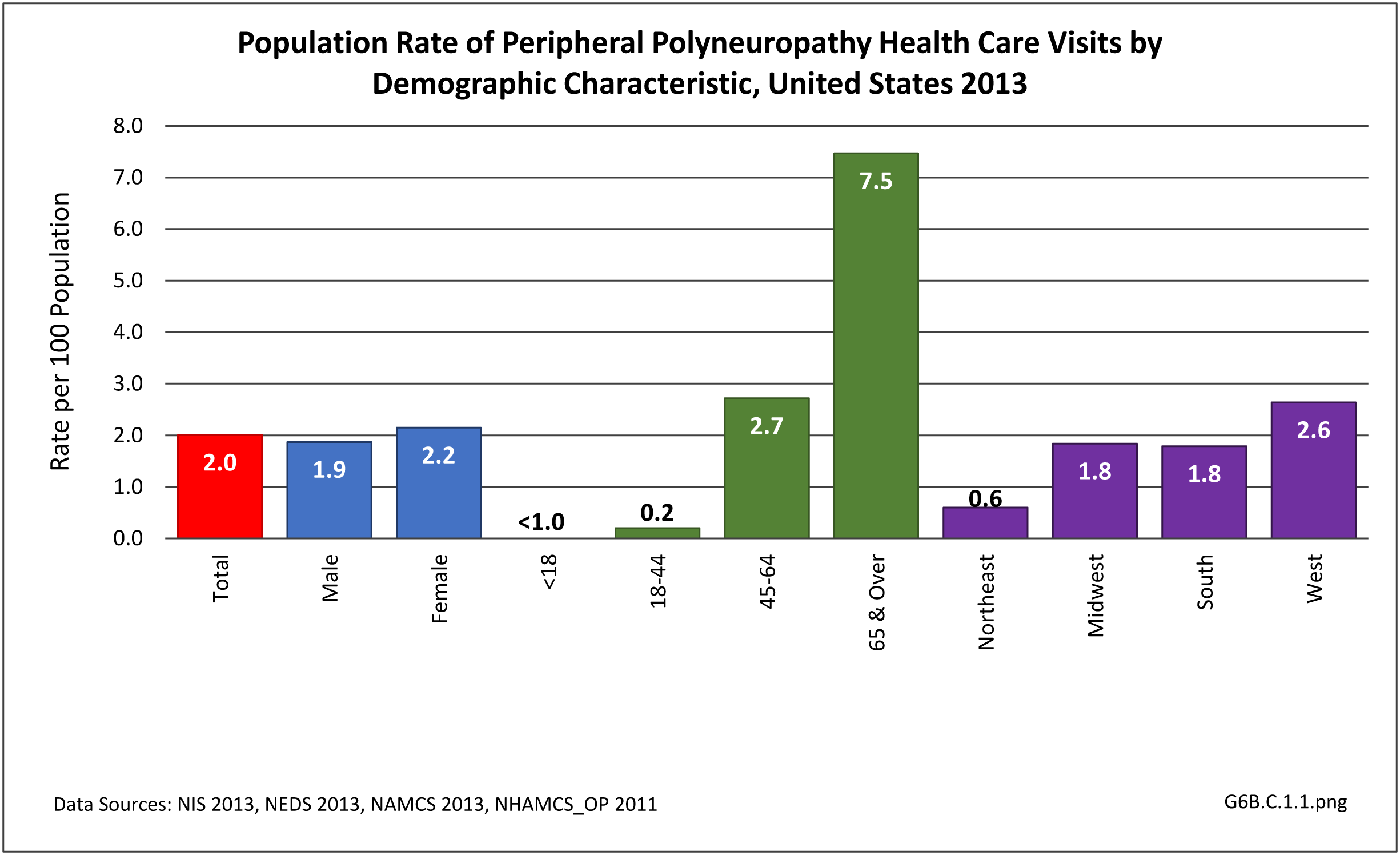
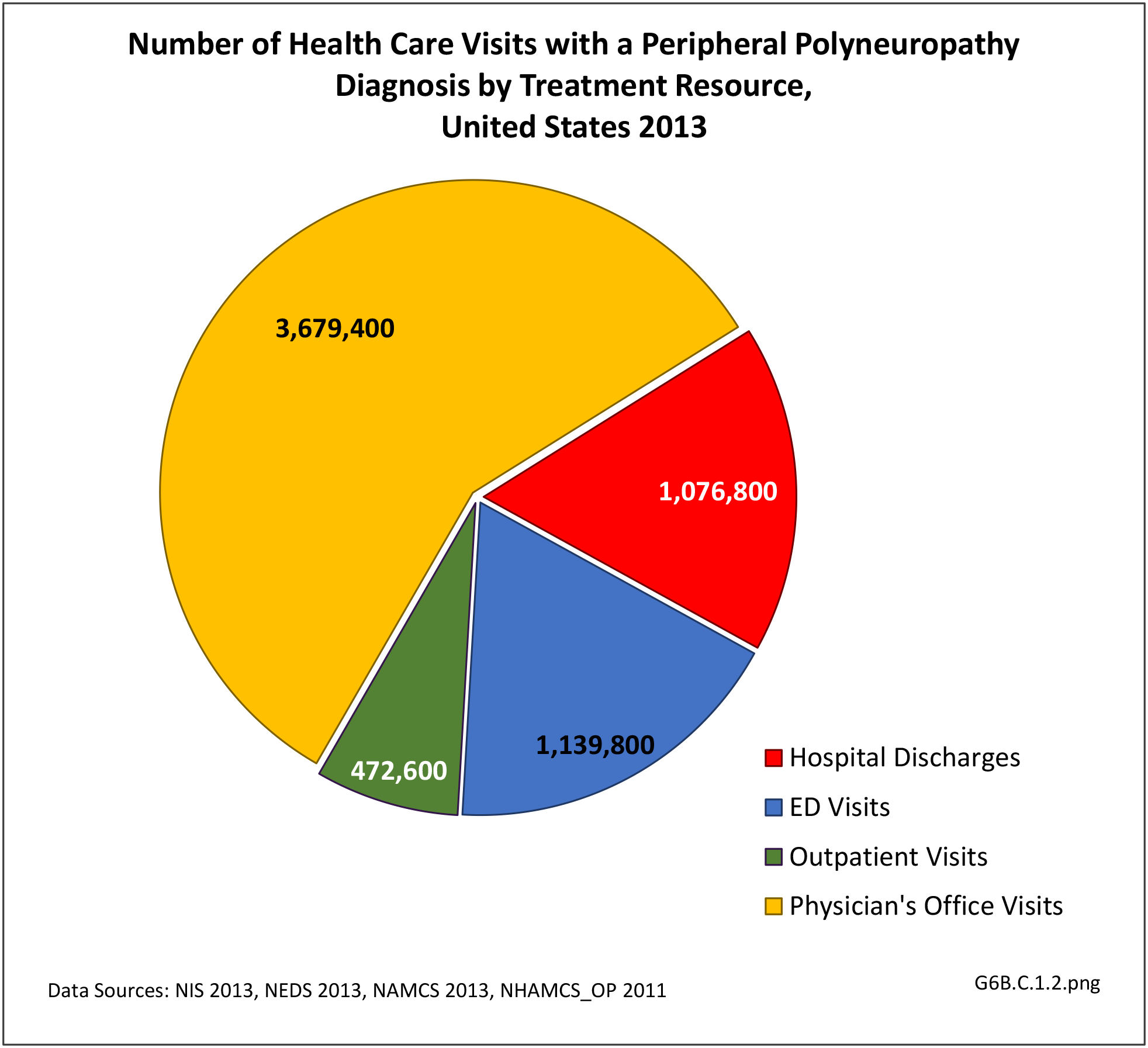
- peripheral neuropathy, involving nerves in the extremity;
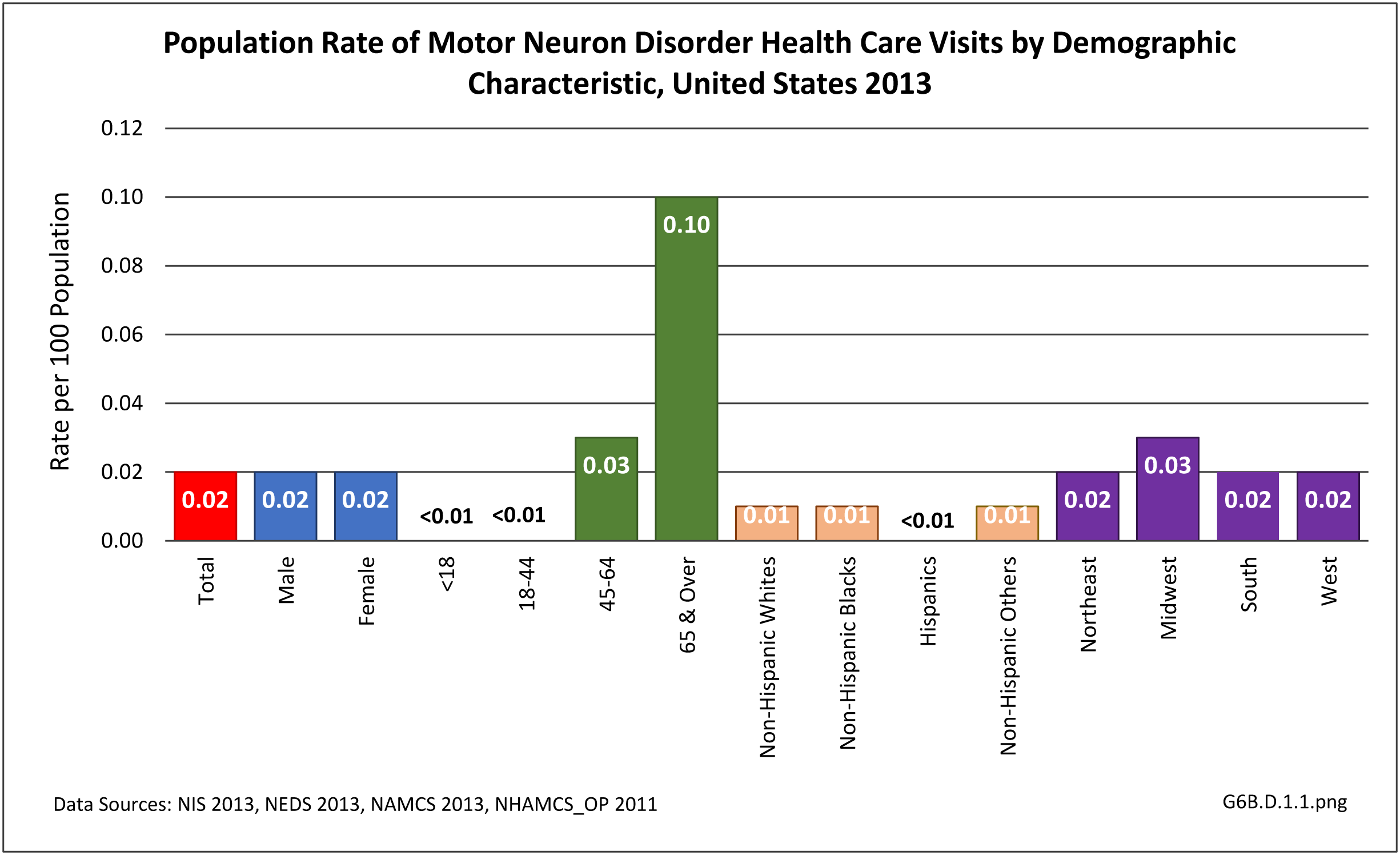
- motor neuron disease, involving motor nerve cells in the spinal cord;
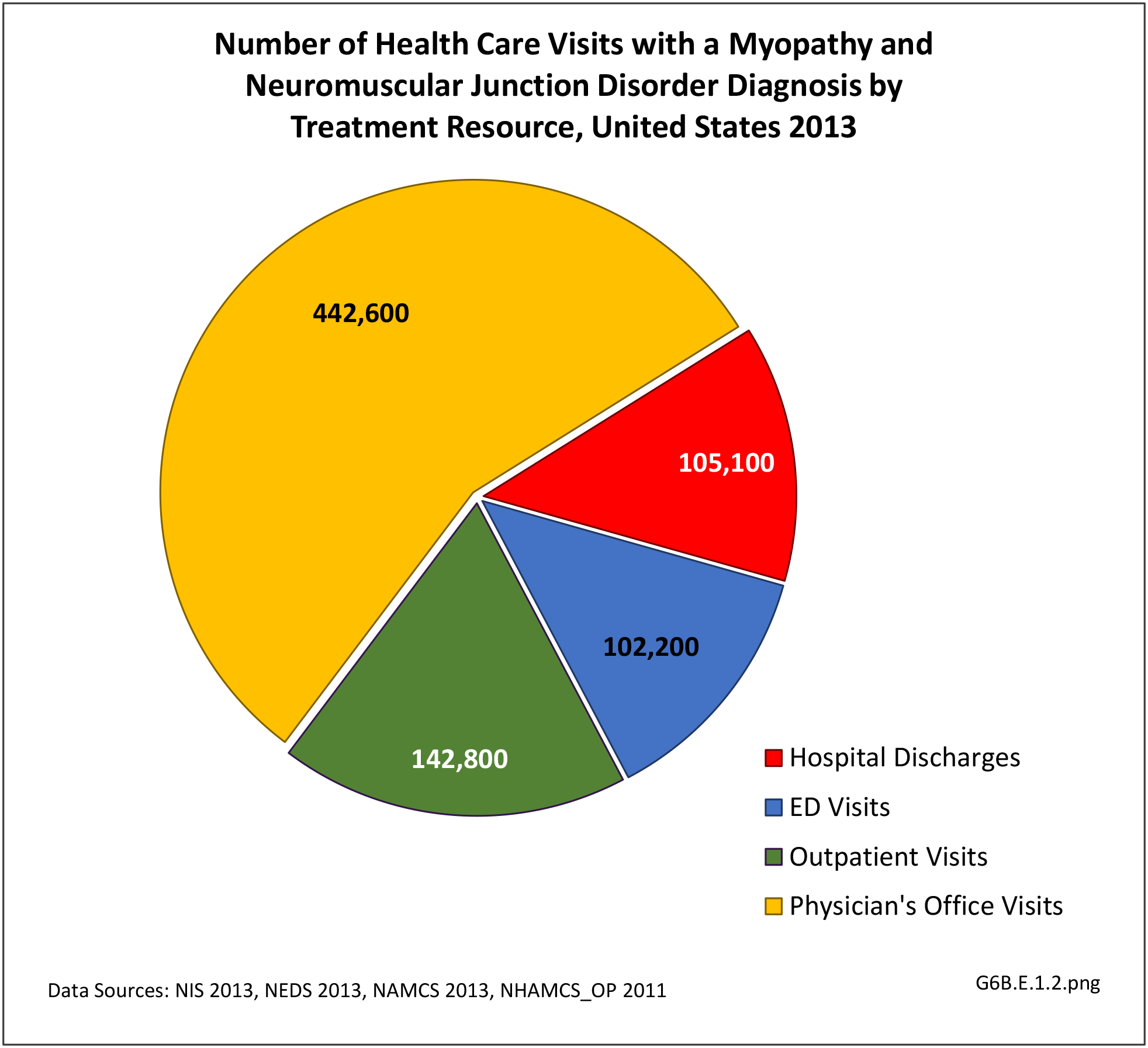
- myopathy and neuromuscular junction disorders, involving muscles and the synapses (contacts) between nerve and muscle; and
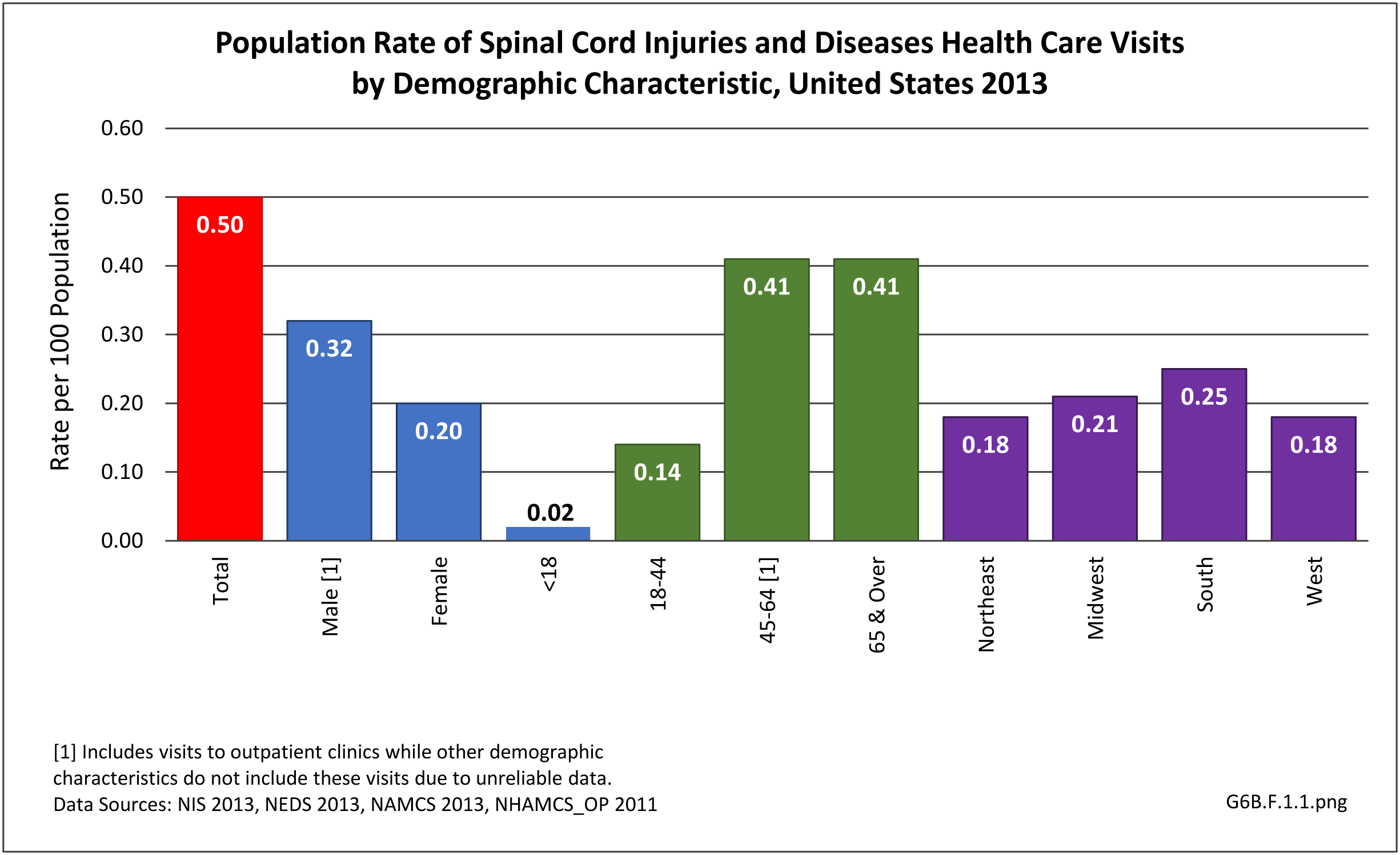
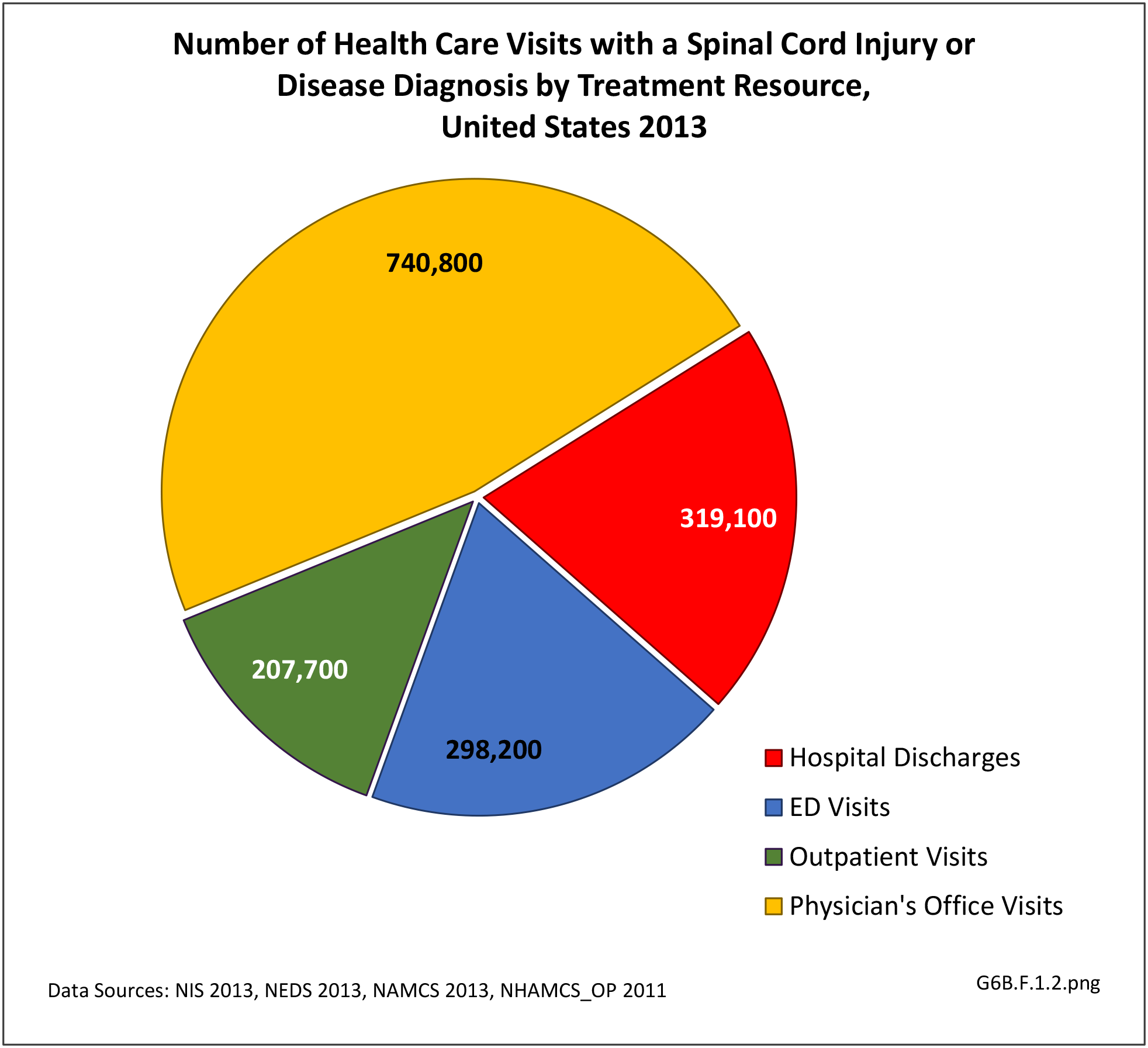
- spinal cord injuries.
Based on the presenting symptoms, NMDs can be classified into disorders with sensory impairment, motor impairment, or both. Neuromuscular disorders can also be categorized roughly into hereditary or acquired neuromuscular NMDs.2 The breakdown of classifications based on the type of impairment at presentation include the following categories.
Sensory Impairment
Sensory impairment can be divided into negative symptoms and positive symptoms. Negative symptoms, which include numbness and loss of joint proprioception with unsteadiness, are often prominent in hereditary conditions such as Charcot Marie Tooth disease or severe neuropathy. Generally, the positive sensory symptoms, such as tingling, pins/needle sensation, and burning pain, are more commonly recognized by patients and the reason they seek medical attention.
Peripheral neuropathy is the most common cause of sensory impairment. It can be divided into hereditary (often related to family history and genetic mutation) and acquired neuropathy. Depending on the area of involvement, neuropathy also can be classified into polyneuropathy, meaning multiple nerves are involved (e.g. distal symmetric polyneuropathy, brachial plexopathy), or mononeuropathy, such as carpal tunnel syndrome, cubital tunnel syndrome, or single level radiculopathies from a disc herniation or spinal stenosis.
The most common acquired polyneuropathy is secondary to diabetes, which affects an estimated 50% of the older type 2 diabetic population.3,4 The most common mononeuropathy is carpal tunnel syndrome (median nerve entrapment at the wrist), followed by ulnar nerve entrapment at the elbow. Charcot Marie Tooth disease is the most common hereditary neuropathy and has variable sensory involvement.
Motor impairment
Motor impairment, manifested as muscle weakness and fatigue, can be secondary to motor neuron disease (such as amyotrophic lateral sclerosis), peripheral neuropathy (involving motor nerves), neuromuscular junction disorders (like myasthenia gravis), and myopathy. When it occurs with sensory impairment, peripheral neuropathy is the most common underlying cause.
Muscle pain (myalgia) or cramps are rare manifestations of some myopathies. Each group of disorders can be further classified depending on the location of involvement and underlying etiology.
Muscle weakness can be due to pain inhibition (from musculoskeletal conditions like arthritis). In contrast to the weakness accompanying pain, the weakness seen with neuromuscular disorders is more profound and often more progressive.
Other motor impairment
Swallowing difficulty (dysphagia), speech problems (dysarthria), and drooping of upper eyelid (ptosis) can be manifestations of muscle weakness in the head and neck secondary to motor neuron disease, myopathy, or neuromuscular disorders.
Mobility impairment and impaired activities of daily living
Mobility involves various types of movement, such as transferring from sitting to standing, walking, and stair/ramp negotiation. Motor impairments involving thigh and hip muscles limit the ability to stand, and can be caused by myopathy or neuropathy (lumbar plexopathy, amyotrophy, radiculopathy). Steady gait requires good balance and joint proprioception (the sense of the relative position of one's own parts of the body and strength of effort being employed in movement), which can be compromised in peripheral neuropathy with sensory impairment. Impairments of sensory and motor nerve functions are important risk factors for falls in older persons and relate directly to disability.5 If the distal muscles that cross the ankle are involved because of peripheral neuropathy or lumbosacral radiculopathy, patients may present with difficulty clearing their foot while walking, resulting in a dragging or slapping gait or “drop foot”.
Upper extremity muscle strength and sensation are important for activities of daily living (ADL), therefore, impairments can cause significant disability. Difficulty with dressing, brushing teeth and combing hair can occur with weakness of the shoulder and arm caused by myopathy, brachial plexopathy or radiculopathy. Injury to the hand and wrist from carpal tunnel syndrome, radiculopathy, motor neuron disease, etc. can lead to dropping objects, difficulty with buttoning and other fine motor skills.
- 1. Dany A, Rapin A, Réveillère C, et al. Exploring quality of life in people with slowly-progressive neuromuscular disease. Disabil Rehabil 2017;39(13):1262-1270. doi: 10.1080/09638288.2016.1191552.
- 2. McDonald CM. Clinical approach to the diagnostic evaluation of hereditary and acquired neuromuscular diseases. Phys Med Rehabil Clin N Am 2012;23(3):495-563.
- 3. Dyck PJ, Katz KM, Karnes JL, Litchy WJ, Klein R, Pach JM: The prevalence by staged severity of various types of diabetic neuropathy, retinopathy and nephropathy in a population-based cohort: The Rochester Diabetic Neuropathy study. Neurology 1993;43:817-824.
- 4. Boulton AJM. Management of diabetic peripheral neuropathy. Clinical Diabetes 2005; 23(1):9-15. https://doi.org/10.2337/diaclin.23.1.9
- 5. Ward RE, Caserotti P, Cauley JA, et al. Mobility-related consequences of reduced lower-extremity peripheral nerve function with age: A systematic review. Aging Dis 2016;7(4):466-78.
Edition:
- Fourth Edition